Clinical presentation of severe hypertriglyceridemia: The signs are clear. Or are they?
Depending on the levels of triglycerides (TGs), patients may or may not have clinical signs or symptoms.
Patients with TG levels ≥500 mg/dL can experience unrecognized, marked increases in triglyceride levels leading to pancreatitis.23
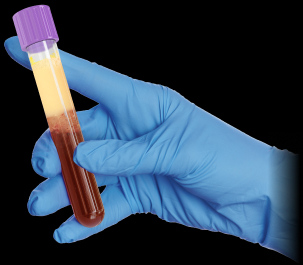
When TG levels increase beyond approximately 750 mg/dL, significant chylomicronemia begins to appear.36 Chylomicronemia presents as a creamy supernatant layer in serum after mild centrifugation and storage of blood samples for 24 hours at 4 degrees C.12