Fasting triglyceride levels ≥880 mg/dL that are refractory to standard triglyceride-lowering therapies
Familial chylomicronemia syndrome (FCS)
FCS is a genetic form of severe hypertriglyceridemia (sHTG) caused by mutations in the gene encoding lipoprotein lipase (LPL) or by mutations in genes encoding proteins necessary for LPL function. This condition manifests in physical complications such as lipemia retinalis, eruptive xanthomas, and an increased risk of potentially life-threatening acute pancreatitis (AP). Read about identifying, diagnosing, and managing FCS.1,2
About FCS
Familial chylomicronemia syndrome (FCS) is an underdiagnosed genetic form of severe hypertriglyceridemia (sHTG)3
Patients with FCS have triglyceride levels that are 10 to 100 times the normal value1,4
FCS is caused by complete or partial deficiency of LPL activity due to mutations in the gene encoding LPL or by mutations in genes encoding proteins necessary for LPL function, leading to the accumulation of very low-density lipoproteins (VLDL) and chylomicrons, leaving individuals with severely elevated triglyceride levels and an increased risk of pancreatitis.1,4
The resulting overabundance of chylomicrons contributes to morbidity
Acute pancreatitis (AP) prevalence as high as 75% has been reported5*
Recurrent pancreatitis rates as high as 48% have been reported6†
Mortality rate for recurrent AP reported to be 6%7‡
Increased risk of organ failure, pancreatic necrosis, and type 3c pancreatogenic diabetes due to chronic pancreatitis8,9
A retrospective review of patients with triglyceride levels >1000 mg/dL with or without a history of acute pancreatitis (N=32) over a median of 44 months. Estimated overall incidence rate of acute pancreatitis of 42 per 1000 person-years in FCS and 13 per 1000 person-years in multifactorial chylomicronemia syndrome (MCS).5
A retrospective study comparing the clinical and biochemical characteristics of patients with genetically confirmed FCS (n=25) or MCS (n=36).6
Survey of lipidologists on the incidence and outcomes of recurrent acute pancreatitis in patients with FCS (N=251).7
apoB-48=apolipoprotein B-48; apoC-III=apolipoprotein C-III; LPL=lipoprotein lipase.
Identifying FCS
The rarity of FCS and overlapping features with MCS—another form of genetic sHTG—often make it difficult to diagnose.11
| Clinical/genetic feature | FCS | MCS |
|---|---|---|
| Triglyceride levels |
Persistently ≥880 mg/dL2
|
Intermittently ≥880 mg/dL2
|
| Response to pharmacologic treatment |
Minimal to no effect (fibrates, niacin, omega-3 fatty acid supplements, and statins)12 |
Variable response (omega-3 fatty acid supplements and niacin)12 |
| Genetic basis |
Can be monogenic13 |
Polygenic6 |
| Age of onset |
Often younger (childhood/adolescence)3,5 |
Often older (mostly adulthood)5 |
| Body weight |
Often within normal body mass index (BMI) range6 |
Often overweight (BMI between 28 and 30 kg/m2)6 |
| Secondary factors |
Less likely (except pregnancy/hormonal birth control)2 |
Likely (metabolic syndrome)2 |
| Population frequency |
1-13 per 1 million people10,13 |
Up to 4000 per 1 million people6 |
Diagnosing FCS
Key clinical features that suggest familial chylomicronemia syndrome (FCS)
Generally, the following should prompt the use of established diagnostic scoring criteria and genetic testing to diagnose FCS2
No known secondary causes for their severe hypertriglyceridemia* (eg, certain conditions or medications)
Recurrent abdominal pain or history of acute pancreatitis
Hypertriglyceridemia can be caused by medications such as glucocorticoids, ethinylestradiol, and neuroleptics, or conditions such as uncontrolled diabetes, hypothyroidism, and pregnancy.2
Diagnostic considerations may include2:

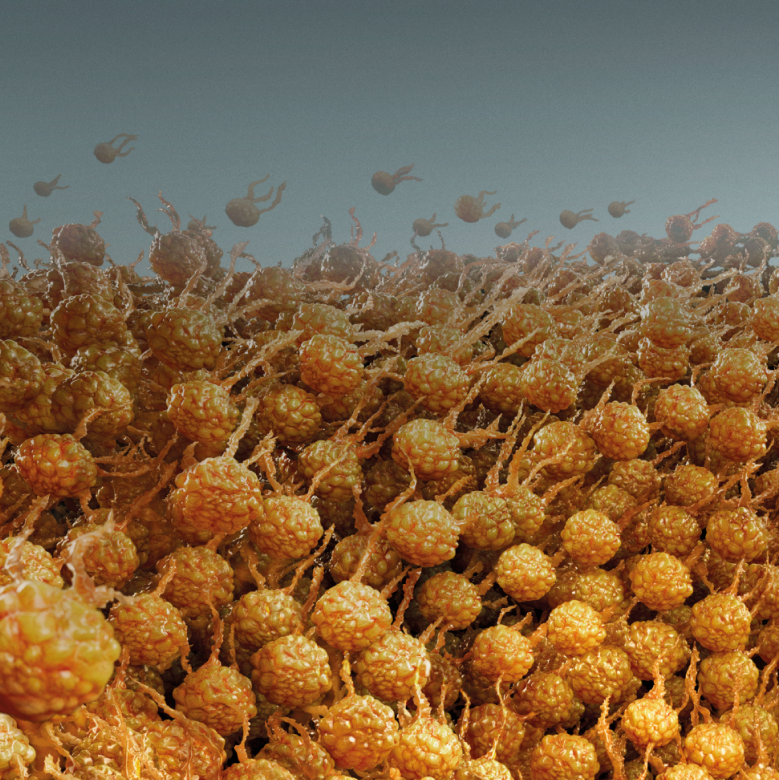
Eruptive xanthomas†

Lipemic blood
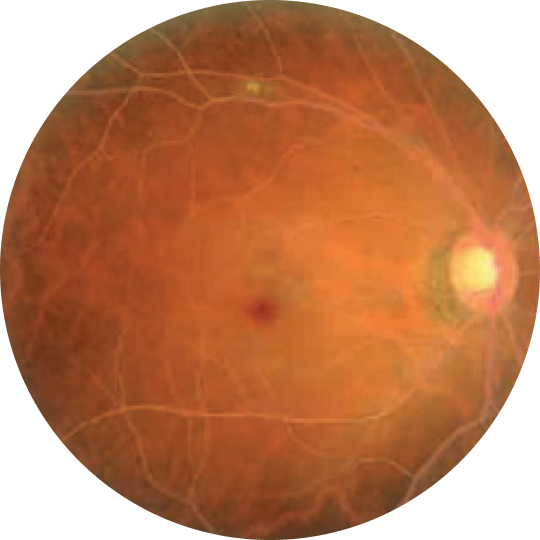
Lipemia retinalis‡
Reprinted with permission from: Abdelghany M, Massoud S. Eruptive xanthoma. Cleve Clin J Med. 2015;82(4)209-210. Copyright © 2024 Cleveland Clinic Foundation. All rights reserved.
Photograph republished from Lai CC, Chang CH. Taiwan J Ophthalmol. 2021;11(4):405-407 under terms of Creative Commons 4.0 License.
Diagnostic scoring tools
Diagnostic scoring tool for familial chylomicronemia syndrome (FCS)
Using the NAFCS scoring criteria to confer a clinical diagnosis
In 2024, the North American FCS (NAFCS) criteria published by Hegele et al were developed and validated specifically for patients in the United States and Canada. This tool uses key clinical features of FCS to generate a score that can help facilitate a diagnosis of FCS.11
This calculator should be used in patients ≥1 year old with hypertriglyceridemia (≥440 mg/dL). In patients ≥10 years old, the calculator is intended for patients who are not responsive to fibrates and high-dose omega-3 fatty acids even when the patient is adherent to therapy (ie, triglycerides do not decrease by 20% or more from these treatments and do not remain reduced).11
Interpreting results
- ≥60 strongly indicates definite FCS
- ≥45 suggests likely FCS rather than MCS
- ≥30-44 suggests patient may have FCS and genetic testing should be considered§
- <30 deemed unlikely to be FCS, but genetic testing may still be needed
Adapted from Hegele RA, Ahmad Z, Ashraf A, et al. Development and validation of clinical criteria to identify familial chylomicronemia syndrome (FCS) in North America. J Clin Lipidol. 2025;19(1):83-94.
The NAFCS Score does not provide a value for pregnant patients.11
Calculator cannot be used for patients <1 year old. If infant presents with no secondary factors that may contribute to hypertriglyceridemia, consider a diagnosis of FCS. If infant presents with ≥1 secondary factor that may contribute to hypertriglyceridemia, but with 2 triglyceride readings >880 mg/dL and unexplained failure to thrive, consider a diagnosis of FCS.11
See the secondary factors table below.11
Further research is needed to determine the validity of a score from 30-44.11
BMI, body mass index; MCS=multifactorial chylomicronemia syndrome.
Genetic testing
Diagnosing familial chylomicronemia syndrome (FCS) with clinical scoring tools and no-cost FCS genetic testing
While clinical scoring tools are available, genetic testing continues to be an important option to support FCS diagnosis, and some payers may require genetic test results.
Because genetic testing can be expensive and may not be available for every patient, Ionis has partnered with PreventionGenetics to provide no-cost testing for eligible patients who:
- Have severe refractory hypertriglyceridemia, defined by a minimum of 2 consecutive fasting triglyceride levels ≥880 mg/dL or 10 mmol/L
- Lack secondary causes or medical conditions known to cause severe hypertriglyceridemia
- Are residents of the United States

FCS patient case
Identifying familial chylomicronemia syndrome (FCS) in your patients
Consider the diagnostic journey and clinical presentation of this hypothetical case study and decide how you would proceed

"It's an awful disease, draining and awful. I'm just so tired of being in the hospital. It takes you away from everything."
Timothy, 25
Severe hypertriglyceridemia (sHTG) and was diagnosed with FCS
- Timothy was first diagnosed with acute pancreatitis (AP) at 19 years of age
- A second episode of AP in his early 20s prompted a deeper assessment by a lipidologist
- A genetic test for common mutations in patients with FCS was indeterminate. However, a clinical diagnosis was conferred based on the North American FCS scoring criteria
"It's an awful disease, draining and awful. I'm just so tired of being in the hospital. It takes you away from everything."
- Timothy was first diagnosed with acute pancreatitis (AP) at 19 years of age
- A second episode of AP in his early 20s prompted a deeper assessment by a lipidologist
- A genetic test for common mutations in patients with FCS was indeterminate. However, a clinical diagnosis was conferred based on the North American FCS scoring criteria
Timothy's clinical presentation
EPA=eicosapentaenoic acid.
Managing FCS
Managing familial chylomicronemia syndrome (FCS): Now there is more than just the mainstay low-fat diet16
FCS treatment has evolved
An FDA-approved prescription medicine is available for adult patients with FCS16
Regardless of treatment, patients must continue to adhere to the recommended FCS diet of <20 grams of fat per day.17 As a reminder, traditional lipid-lowering treatments are insufficient for reducing triglyceride levels in patients with FCS due to these patients’ lack of lipoprotein lipase activity.14,18
References
References
-
Ginsberg HN, Packard CJ, Chapman MJ, et al. Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies—a consensus statement from the European Atherosclerosis Society. Eur Heart J. 2021;42(47):4791-4806.
-
Moulin P, Dufour R, Averna M, et al. Identification and diagnosis of patients with familial chylomicronaemia syndrome (FCS): expert panel recommendations and proposal of an "FCS score". Atherosclerosis. 2018;275:265-272.
-
Davidson M, Stevenson M, Hsieh A, et al. The burden of familial chylomicronemia syndrome: results from the global IN-FOCUS study. J Clin Lipidol. 2018;12(4):898-907.e2.
-
Gaudet D, Brisson D, Tremblay K, et al. Targeting APOC3 in the familial chylomicronemia syndrome. N Engl J Med. 2014;371(23):2200-2206.
-
D’Erasmo L, Di Costanzo A, Cassandra F, et al. Spectrum of mutations and long-term clinical outcomes in genetic chylomicronemia syndromes. Arterioscler Thromb Vasc Biol. 2019;39(12):2531-2541.
-
Paquette M, Bernard S. The evolving story of multifactorial chylomicronemia syndrome. Front Cardiovasc Med. 2022;9:886266.
-
Gaudet D, Blom D, Bruckert E, et al. Acute pancreatitis is highly prevalent and complications can be fatal in patients with familial chylomicronemia: results from a survey of lipidologist. J Clin Lipidol. 2016;10(3):680-681. National Lipid Association 2016 Scientific Sessions abstract 136.
-
Nawaz H, Koutroumpakis E, Easler J, et al. Elevated serum triglycerides are independently associated with persistent organ failure in acute pancreatitis. Am J Gastroenterol. 2015;110(10):1497-1503.
-
Shemesh E, Zafrir B. Hypertriglyceridemia-related pancreatitis in patients with type 2 diabetes: links and risks. Diabetes Metab Syndr Obes. 2019;12:2041-2052.
-
O'Dea LSL, MacDougall J, Alexander VJ, et al. Differentiating familial chylomicronemia syndrome from multifactorial severe hypertriglyceridemia by clinical profiles. J Endocr Soc. 2019;3(12):2397-2410.
-
Hegele RA, Ahmad Z, Ashraf A, et al. Development and validation of clinical criteria to identify familial chylomicronemia syndrome (FCS) in North America. J Clin Lipidol. 2025;19(1):83-94.
-
Brahm AJ, Hegele RA. Chylomicronaemia—current diagnosis and future therapies. Nat Rev Endocrinol. 2015;11(6):352-362.
-
Pallazola VA, Sajja A, Derenbecker R, et al. Prevalence of familial chylomicronemia syndrome in a quaternary care center. Eur J Prev Cardiol. 2020;27(19):2276-2278.
-
Chyzhyk V, Brown AS. Familial chylomicronemia syndrome: a rare but devastating autosomal recessive disorder characterized by refractory hypertriglyceridemia and recurrent pancreatitis. Trends Cardiovasc Med. 2020;30(2):80-85.
-
Hegele RA, Ahmad Z, Ashraf A, et al. Development and validation of clinical criteria to identify familial chylomicronemia syndrome (FCS) in North America. J Clin Lipidol. 2025;19(1)(online-only supplementary material):83-94.
-
Olezarsen. Prescribing information. Ionis Pharmaceuticals.
-
Williams L, Rhodes KS, Karmally W, et al. Familial chylomicronemia syndrome: bringing to life dietary recommendations throughout the life span. J Clin Lipidol. 2018;12(4):908-919.
-
Baass A, Paquette M, Bernard S, Hegele RA. Familial chylomicronemia syndrome: an under-recognized cause of severe hypertriglyceridaemia. J Intern Med. 2020;287(4):340-348.