Understanding the pathophysiology
of triglyceride disorders
Dysregulation of triglyceride-rich lipoproteins can lead to increased
health risks.
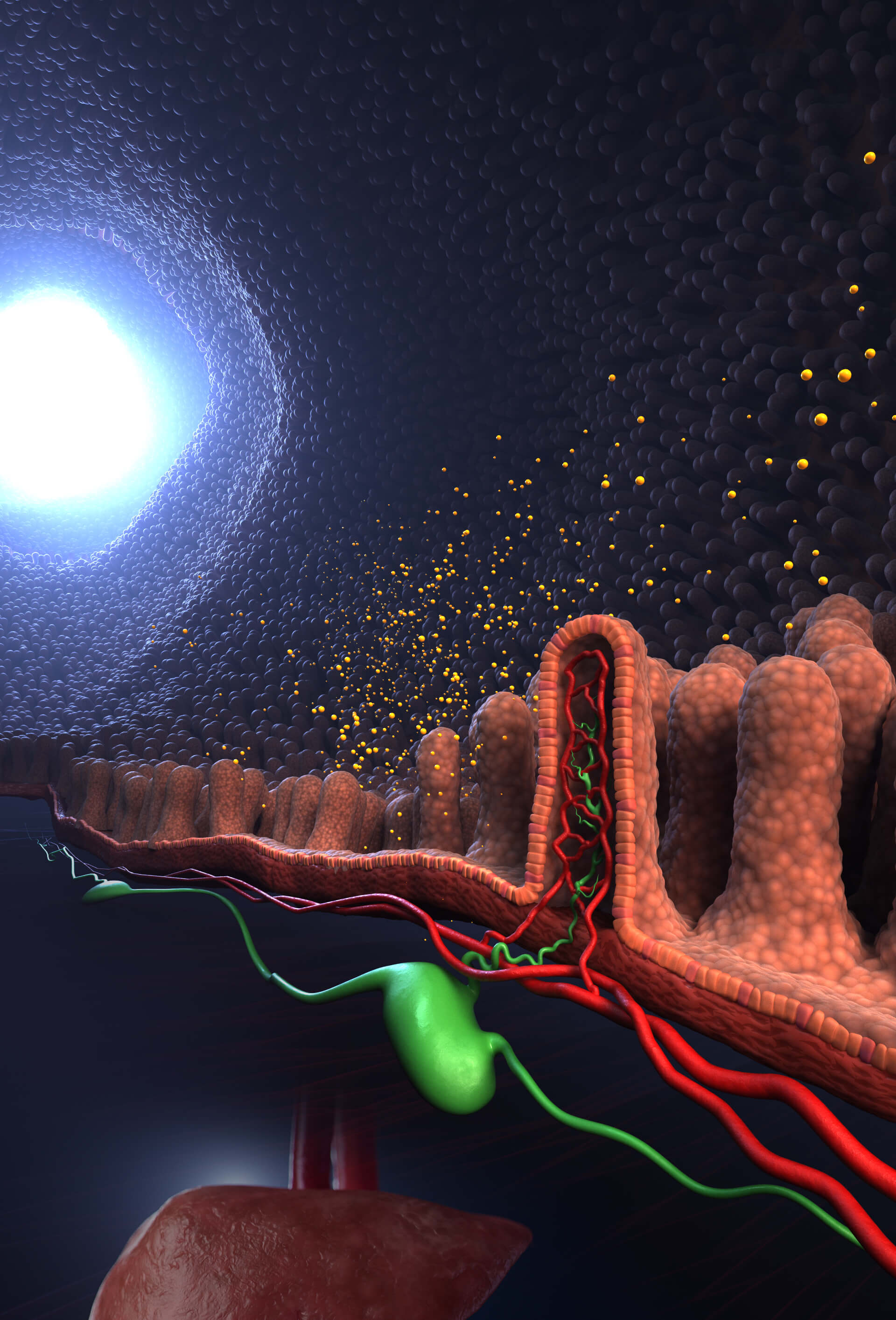
Triglyceride-rich lipoproteins (TRLs) transport triglycerides (TGs) from the intestines and liver to peripheral tissues for energy utilization or storage. Triglyceride disorders typically feature overproduction or decreased clearance of TRLs, which leads to elevated triglyceride levels in the blood.1
Genetic factors, lifestyle factors (such as diet and physical inactivity), or secondary conditions (like diabetes mellitus and obesity) may cause this imbalance.1,4
The accumulation of TRLs and their remnants in the circulation increases the risk of developing acute pancreatitis and cardiovascular disease by promoting atherogenesis, inflammation, and endothelial dysfunction.1
Explore the pathophysiology of triglyceride disorders below.
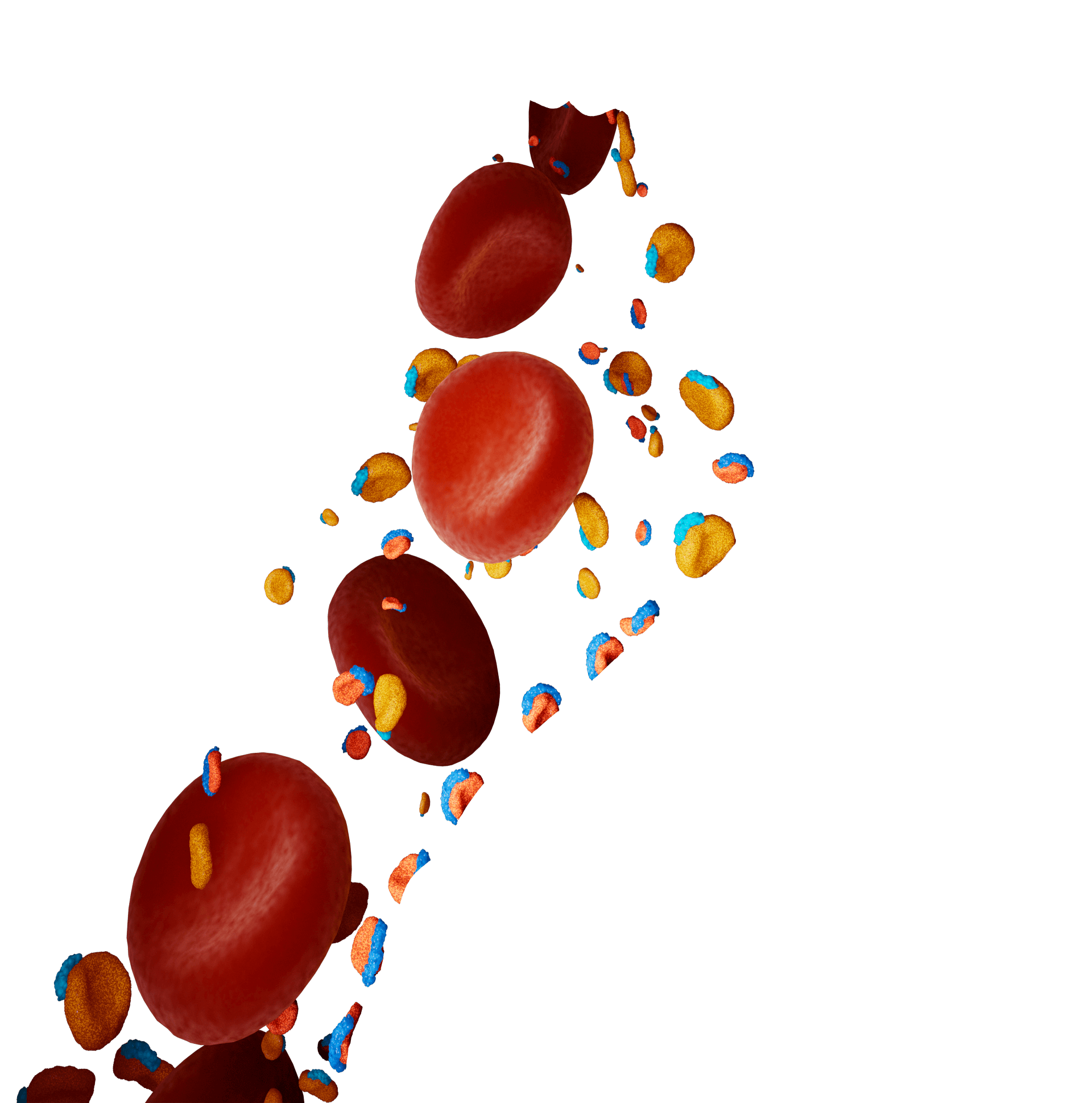
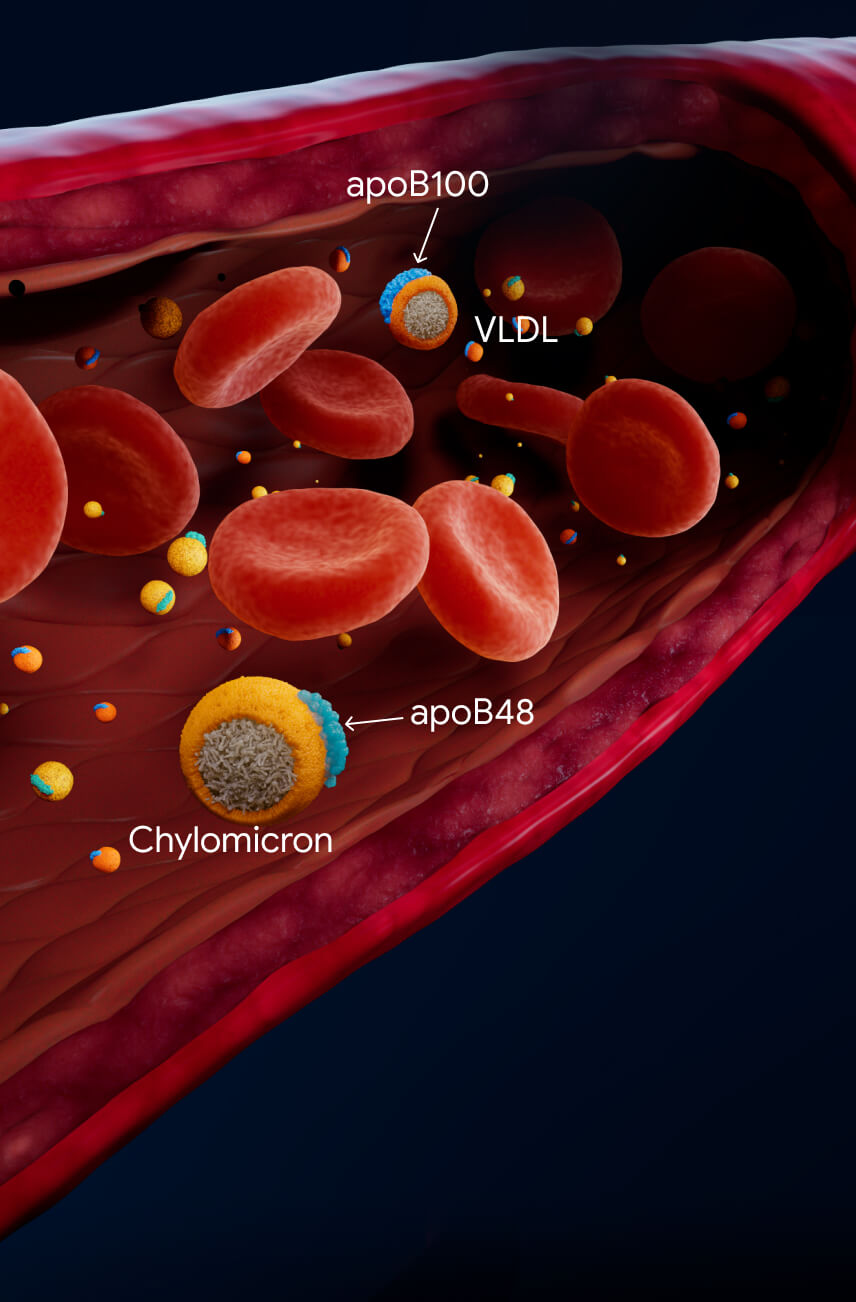
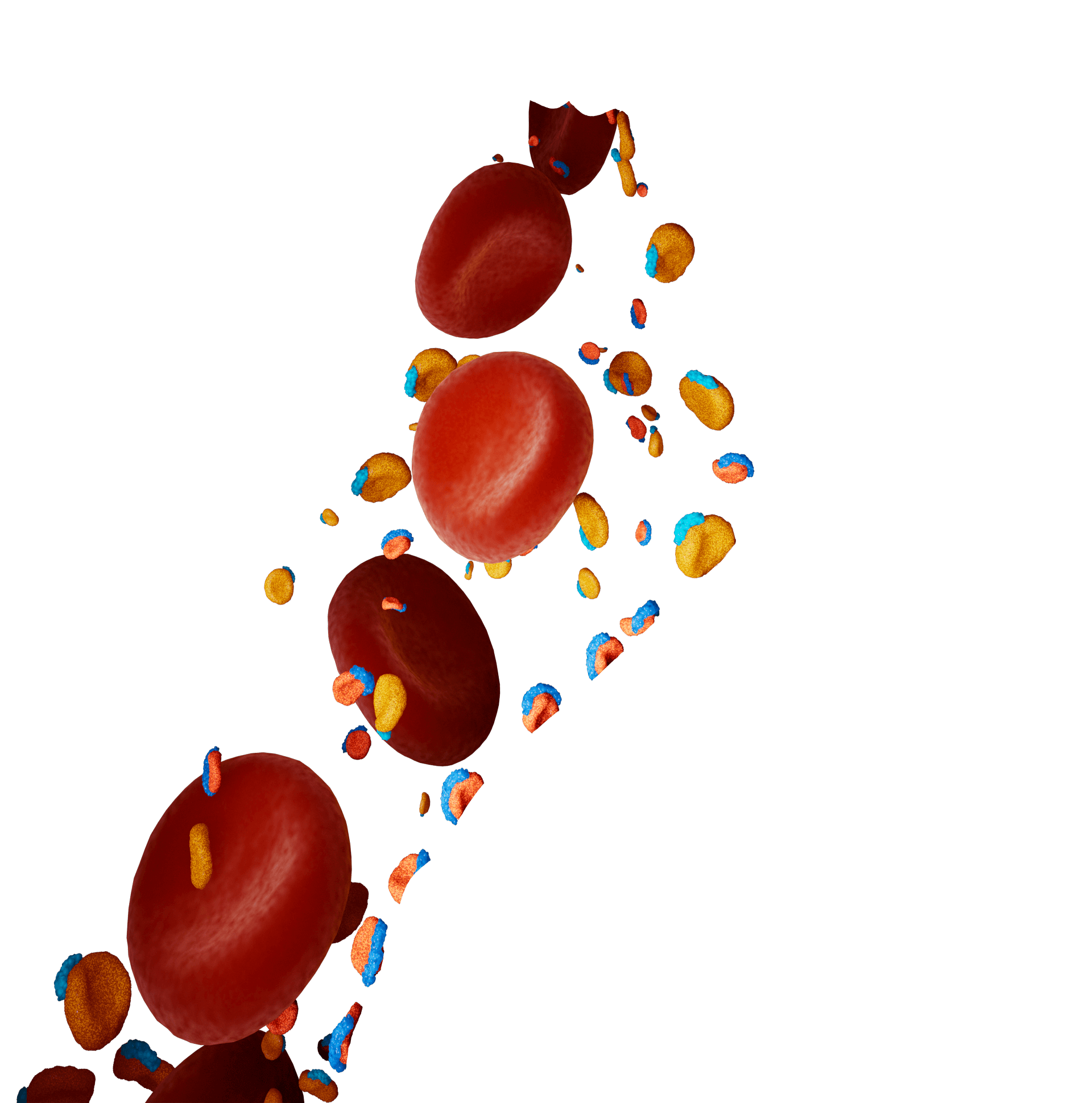
The main TRLs in the blood are chylomicrons and very-low-density lipoproteins
(VLDL).1,4
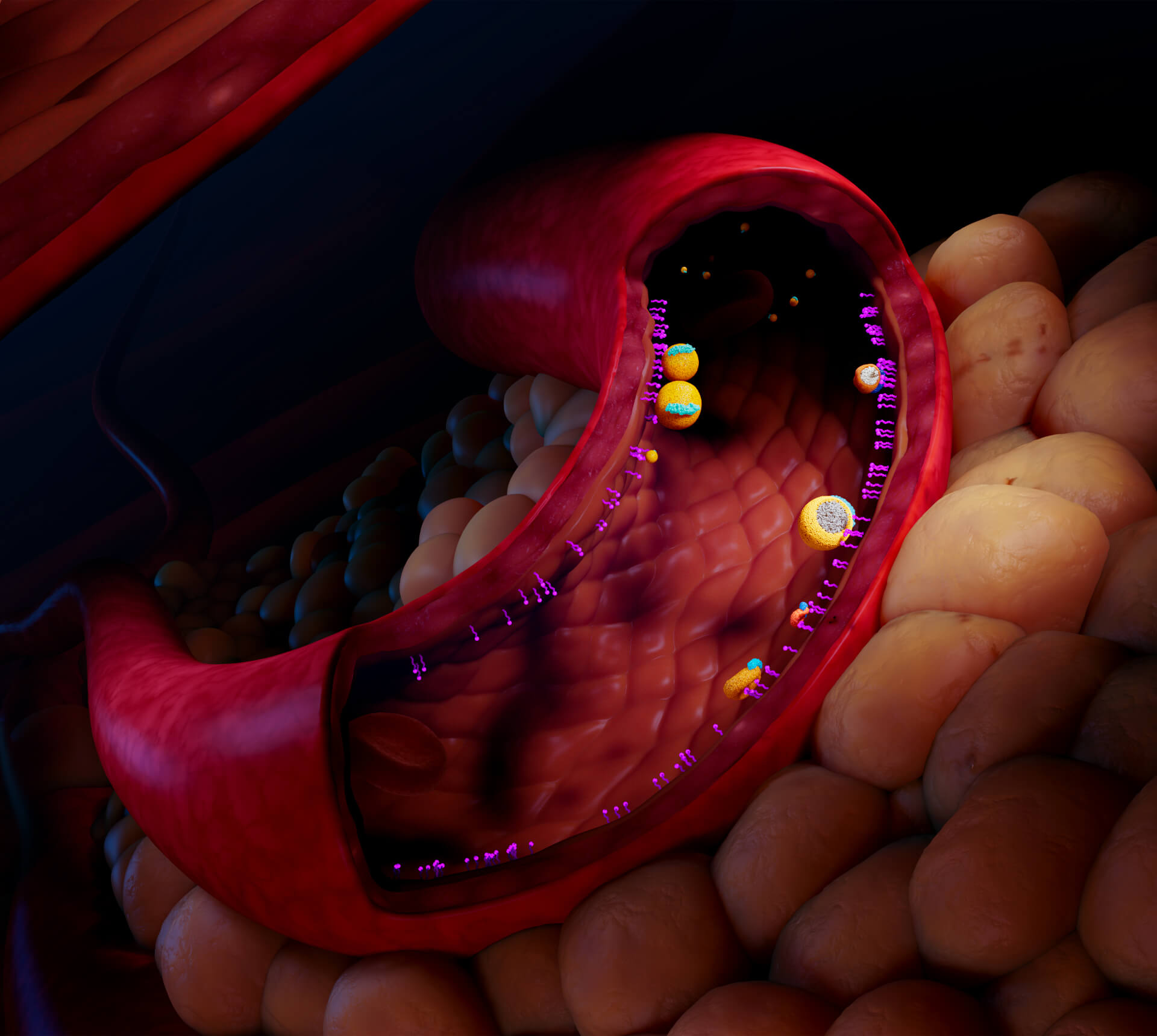
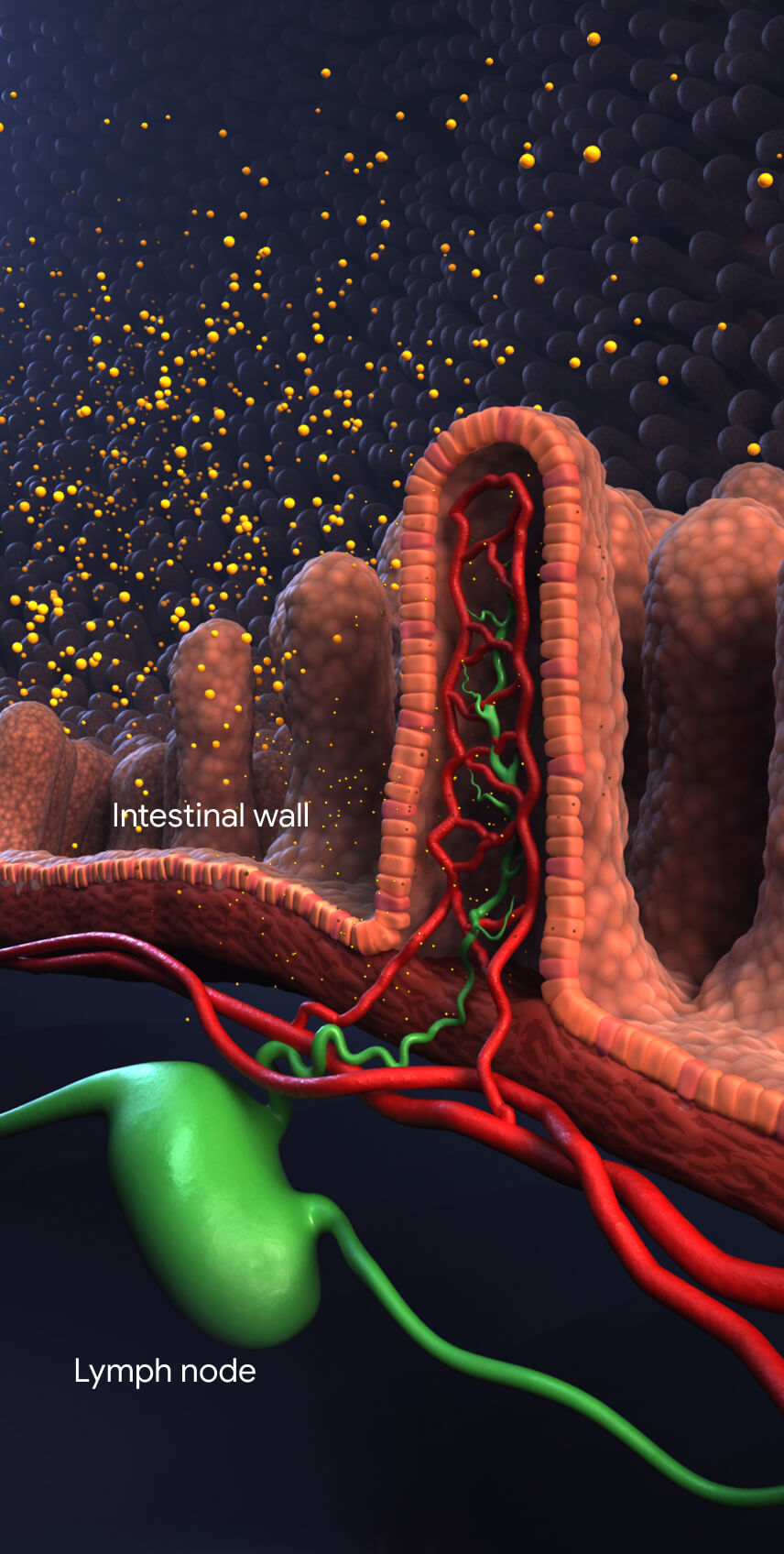
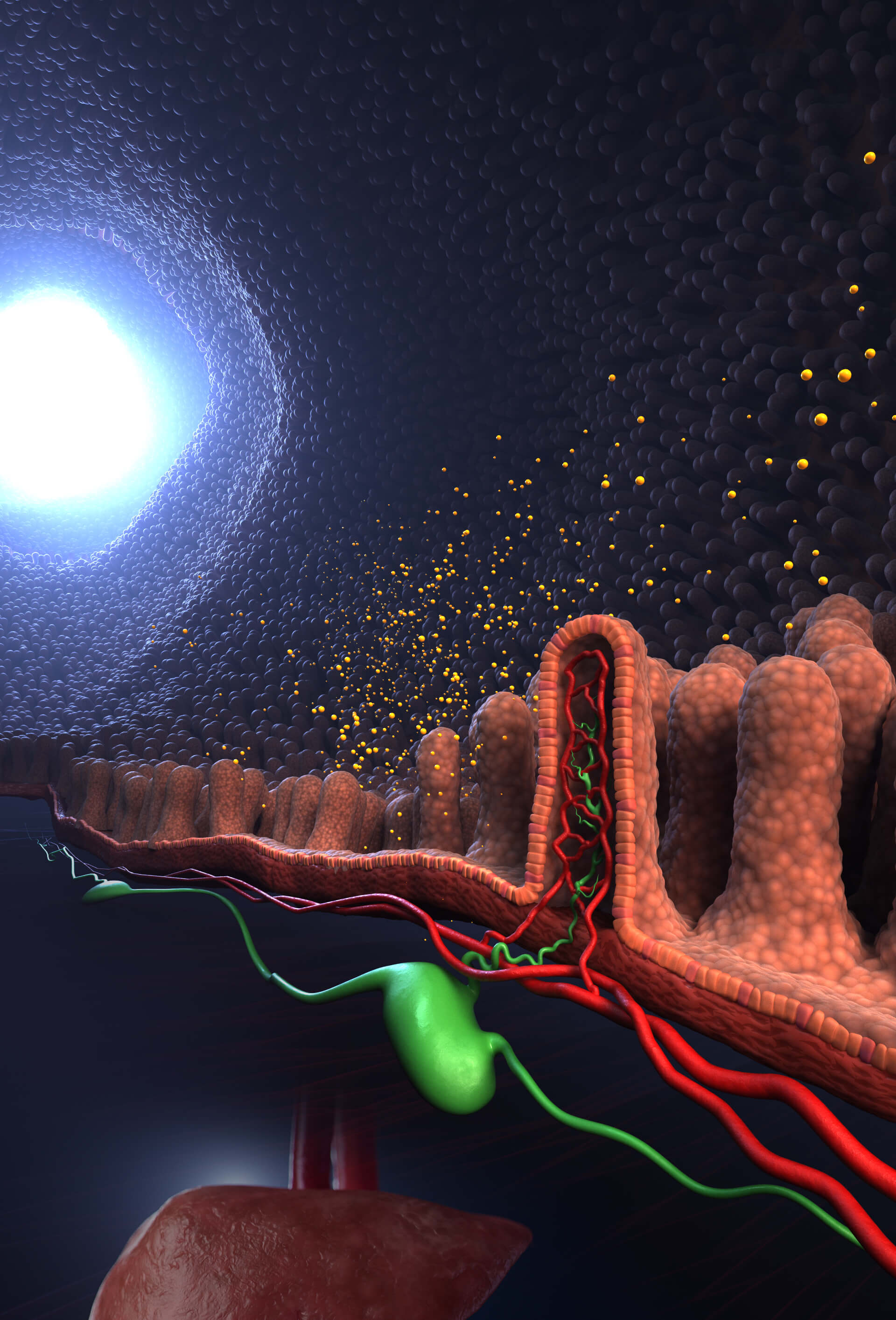
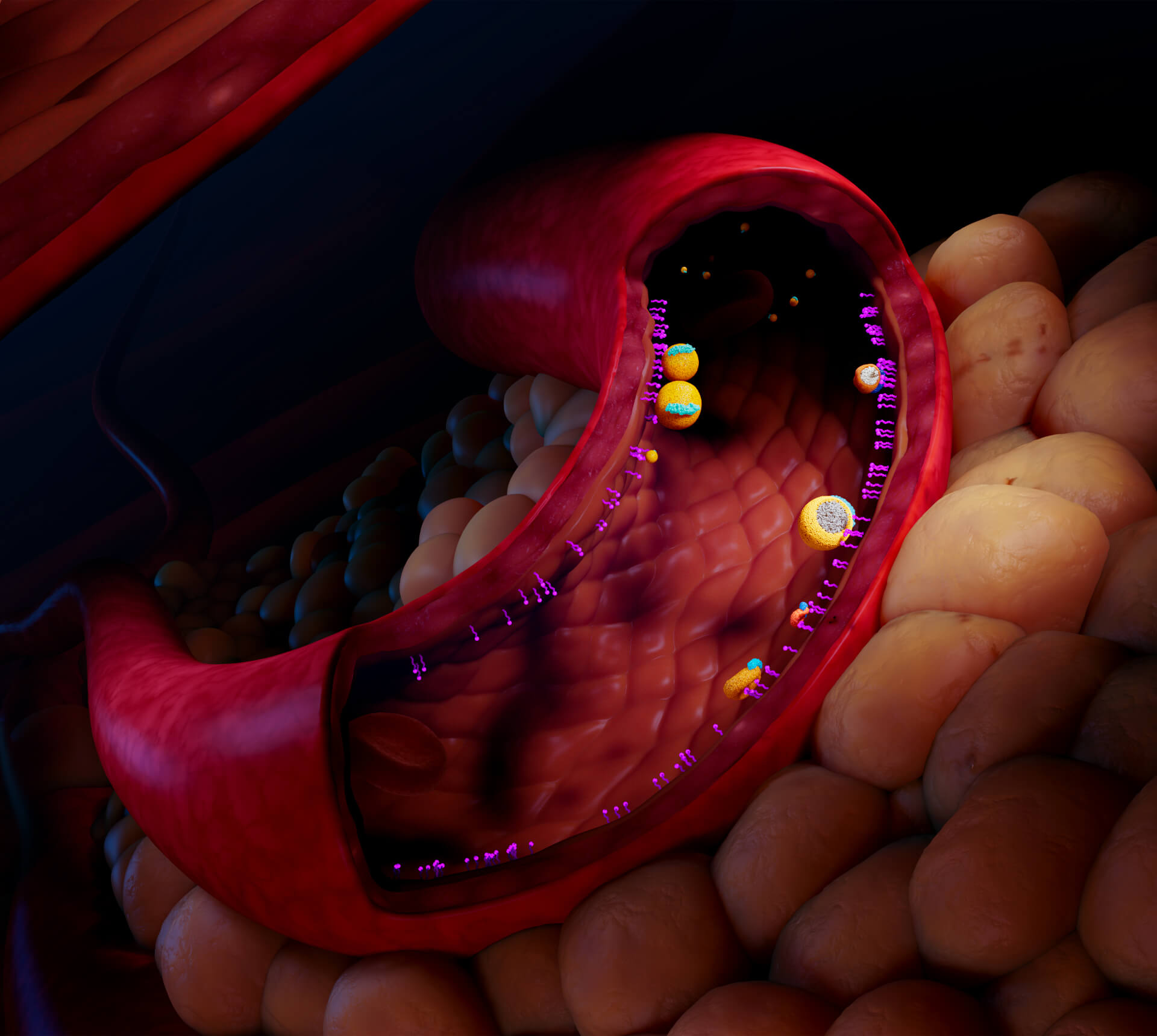
Intestinal wall
Chylomicrons are synthesized from dietary fats by intestinal enterocytes. They enter
the bloodstream through the lymphatic system.14,16
Lymph node

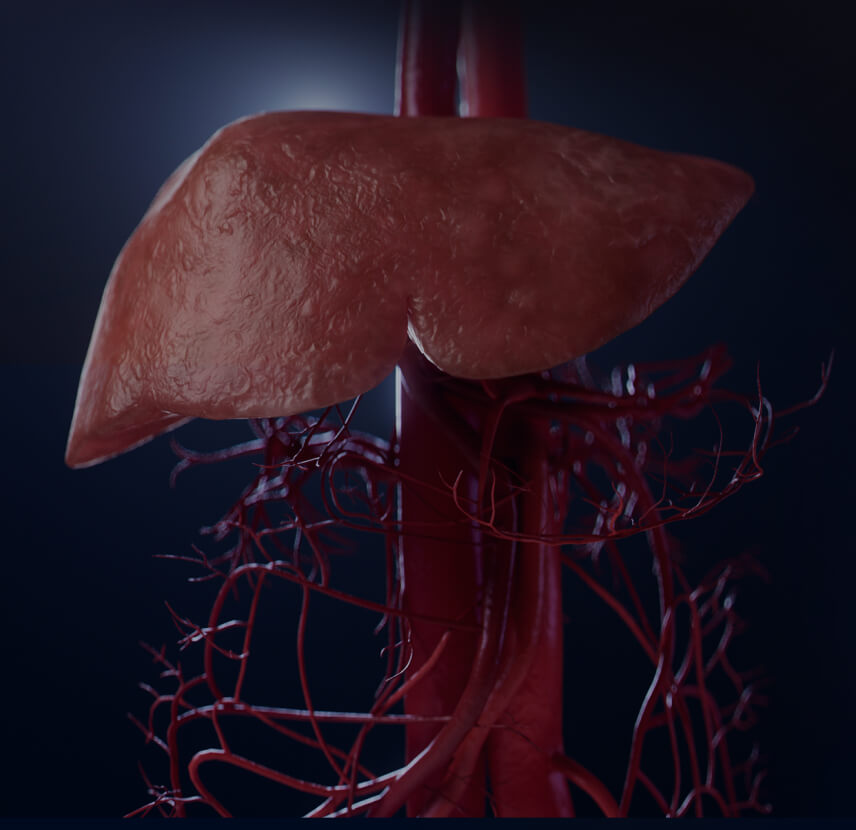
VLDL are made in the liver and secreted directly into the bloodstream.4
apoB100
VLDL
apoB48
Chylomicron
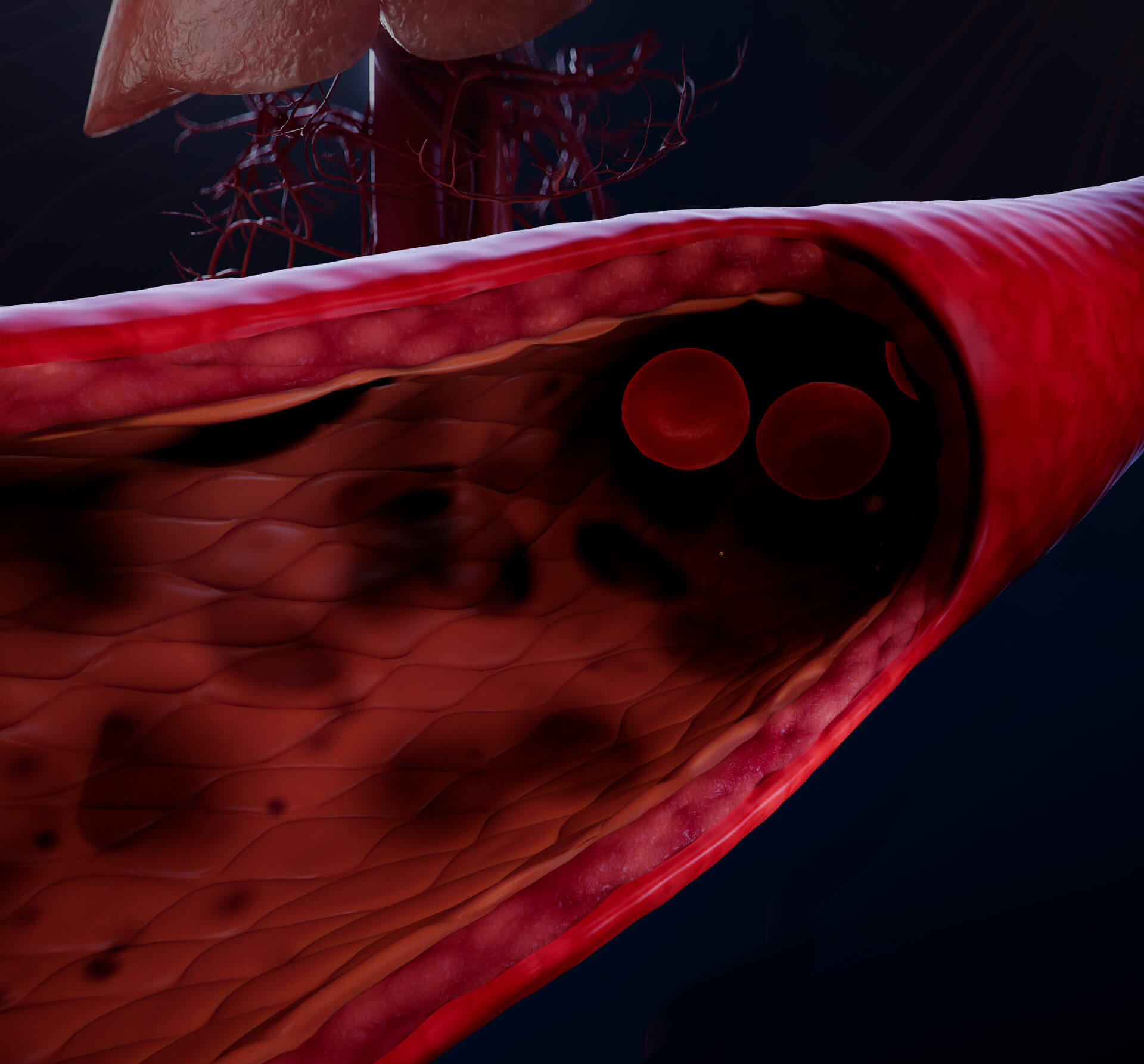
Chylomicrons and VLDL transport triglycerides in the bloodstream.1
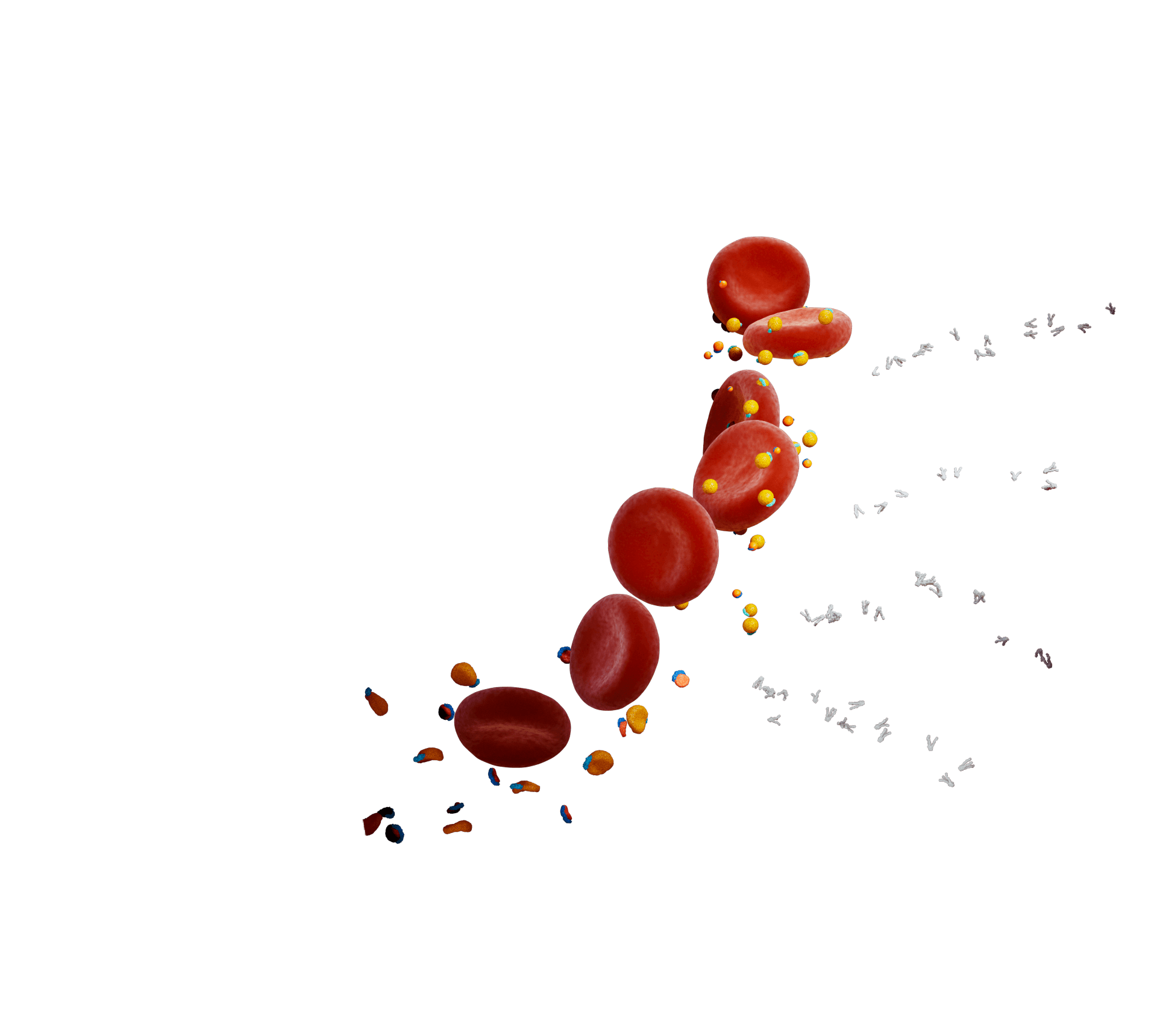
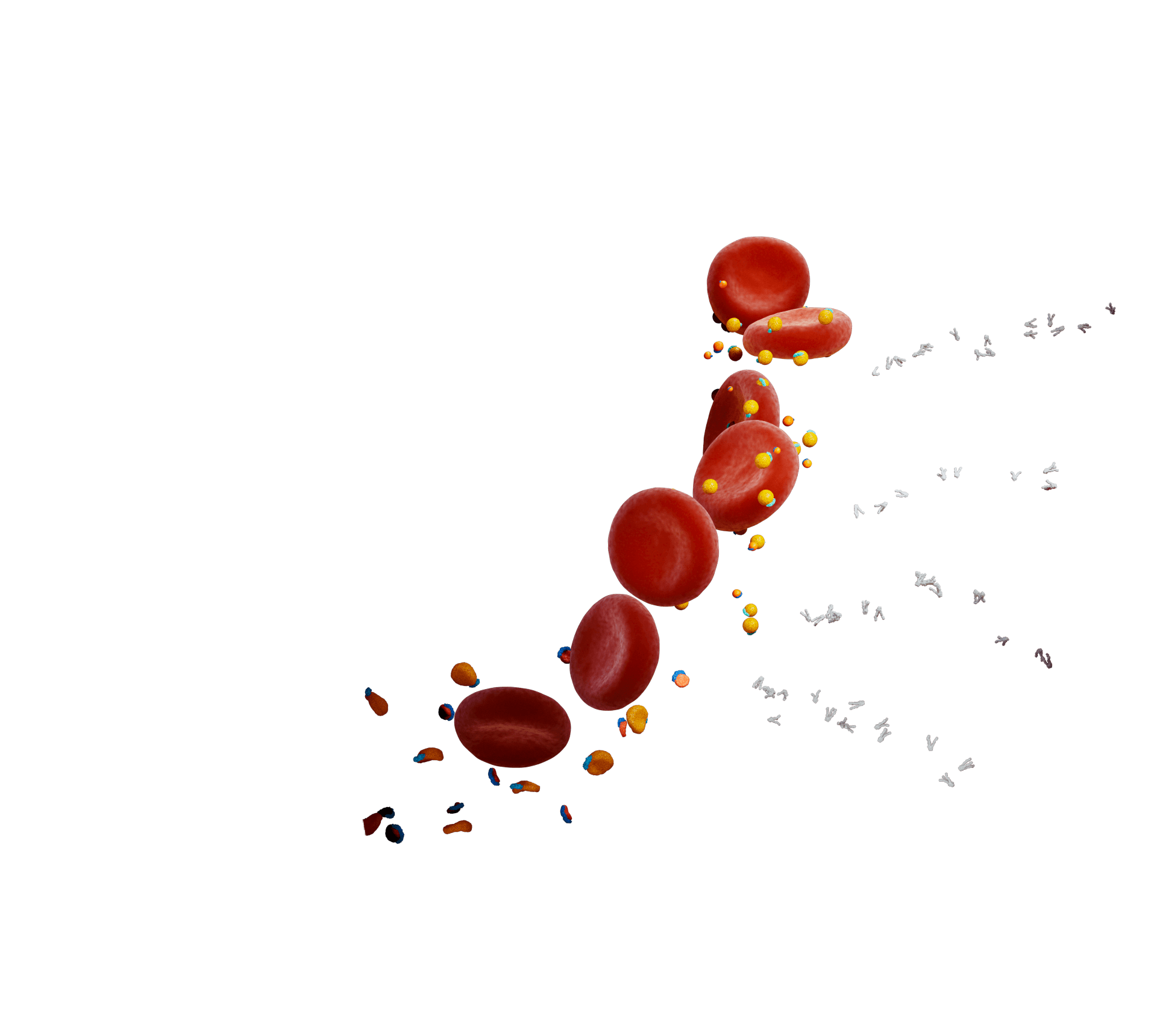
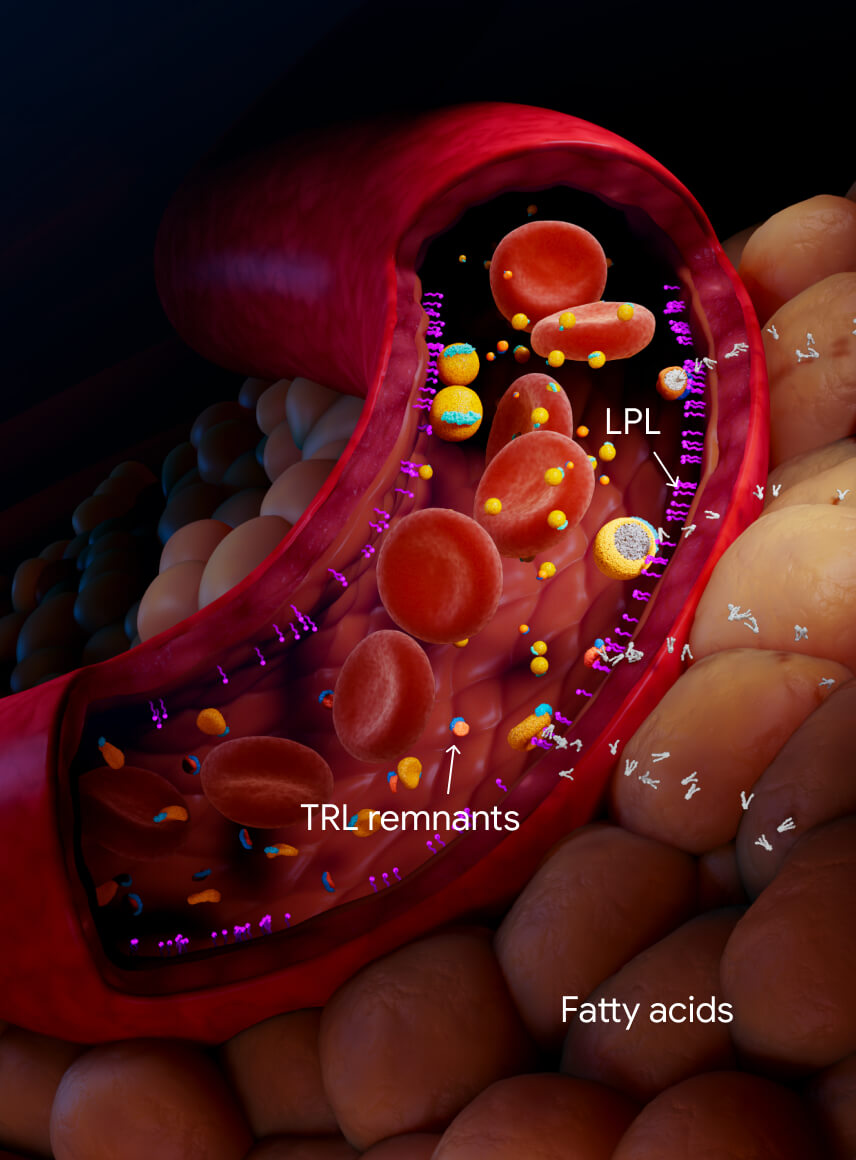
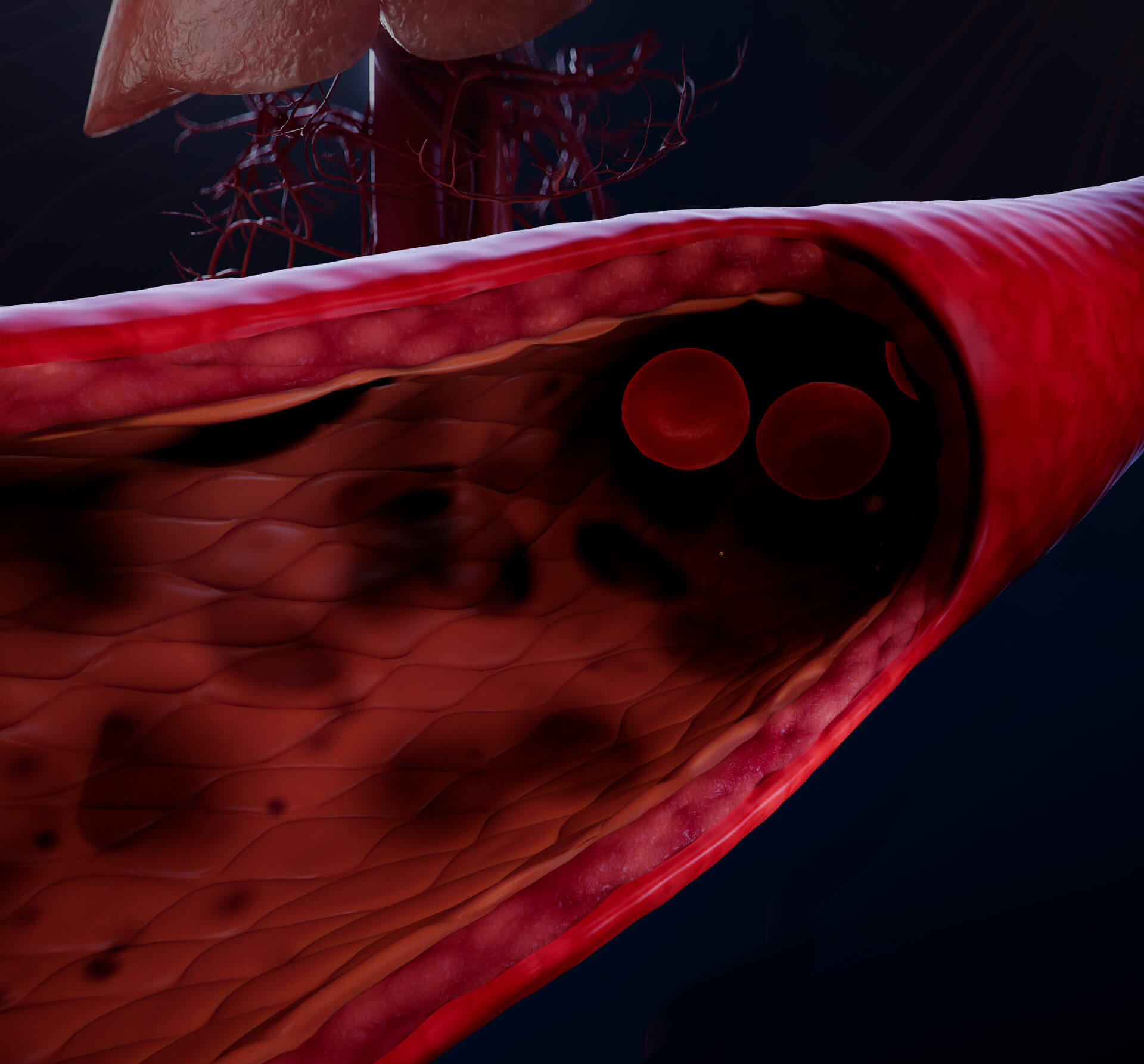
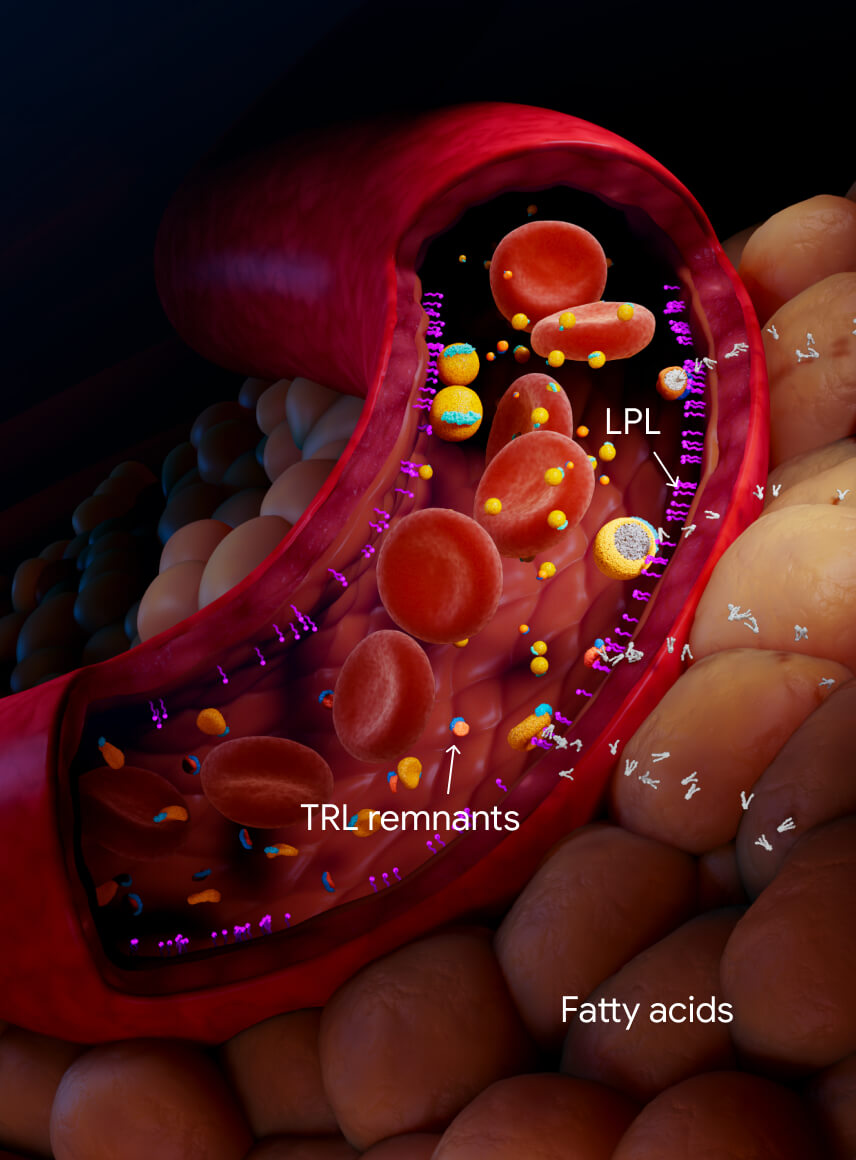
In muscle and adipose tissues, endothelial cells express lipoprotein lipase (LPL) on their
surface.16
LPL
TG lipolysis mediated by LPL usually clears chylomicrons from the bloodstream within 3-4 hours
after a meal.1,16 LPL also lipolyzes TGs from VLDL leaving TRL remnant particles,
intermediate-density lipoproteins (IDL), and small, dense low-density lipoproteins (LDL).1
Fatty acids
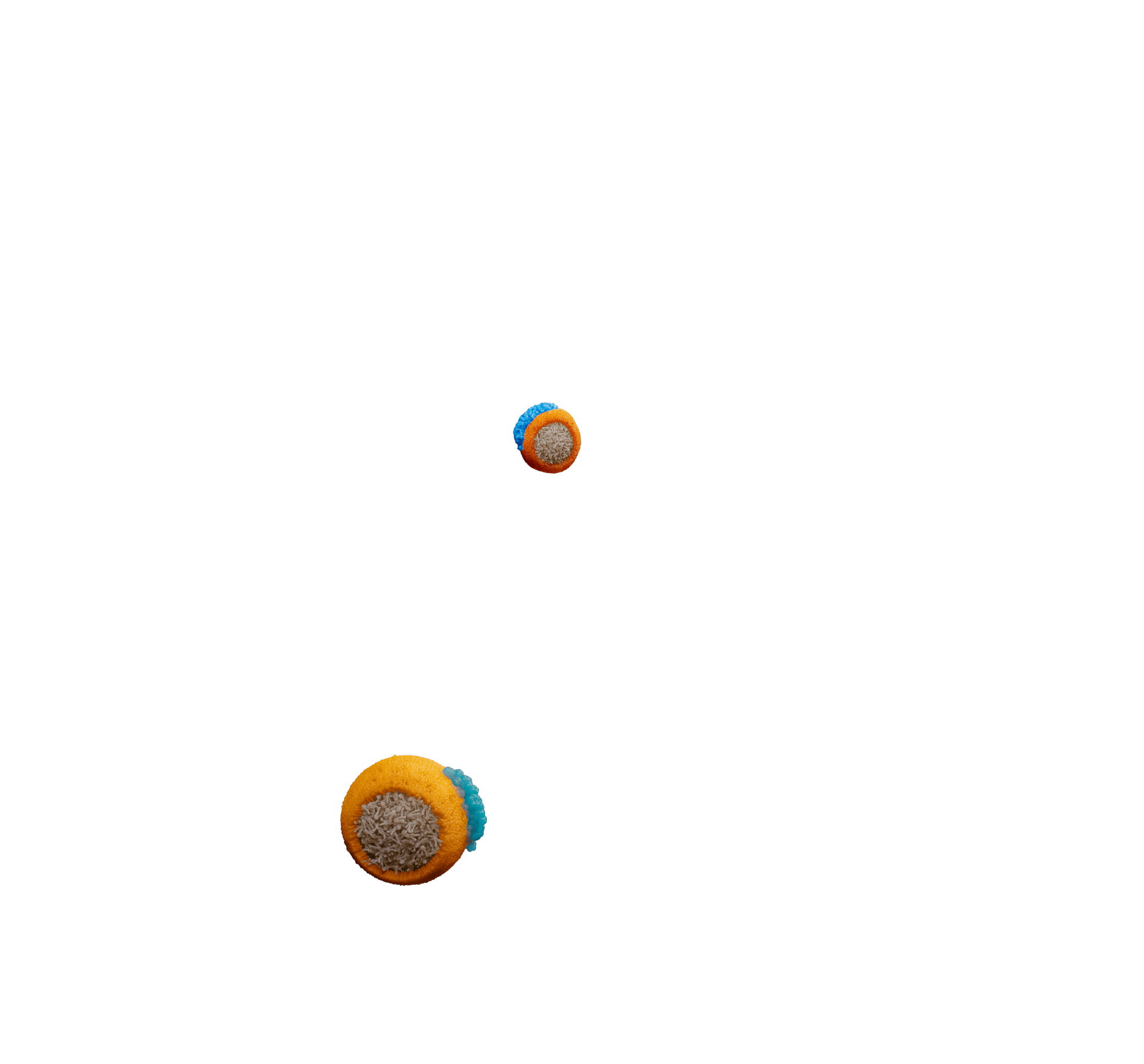
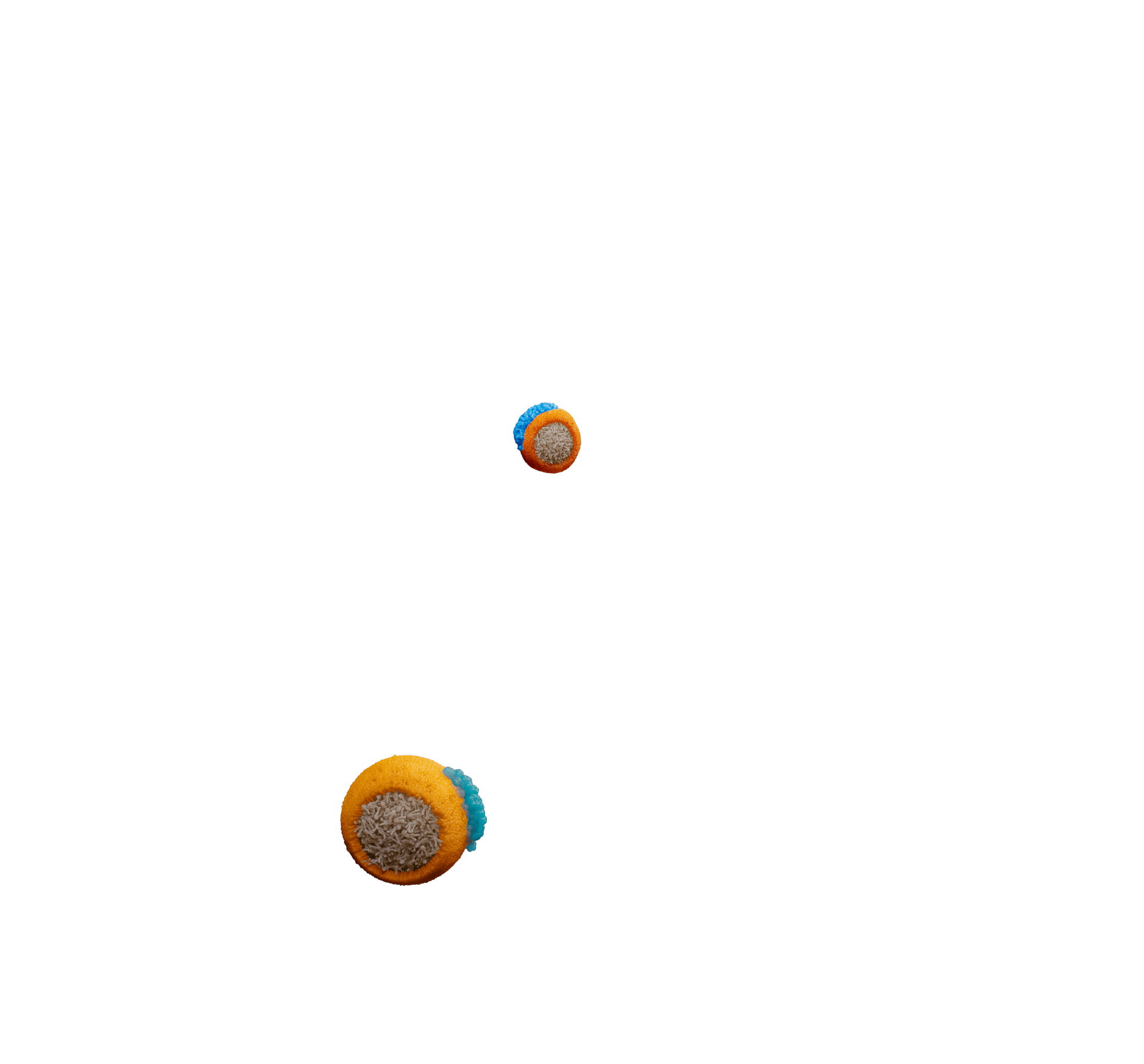
TRL remnants
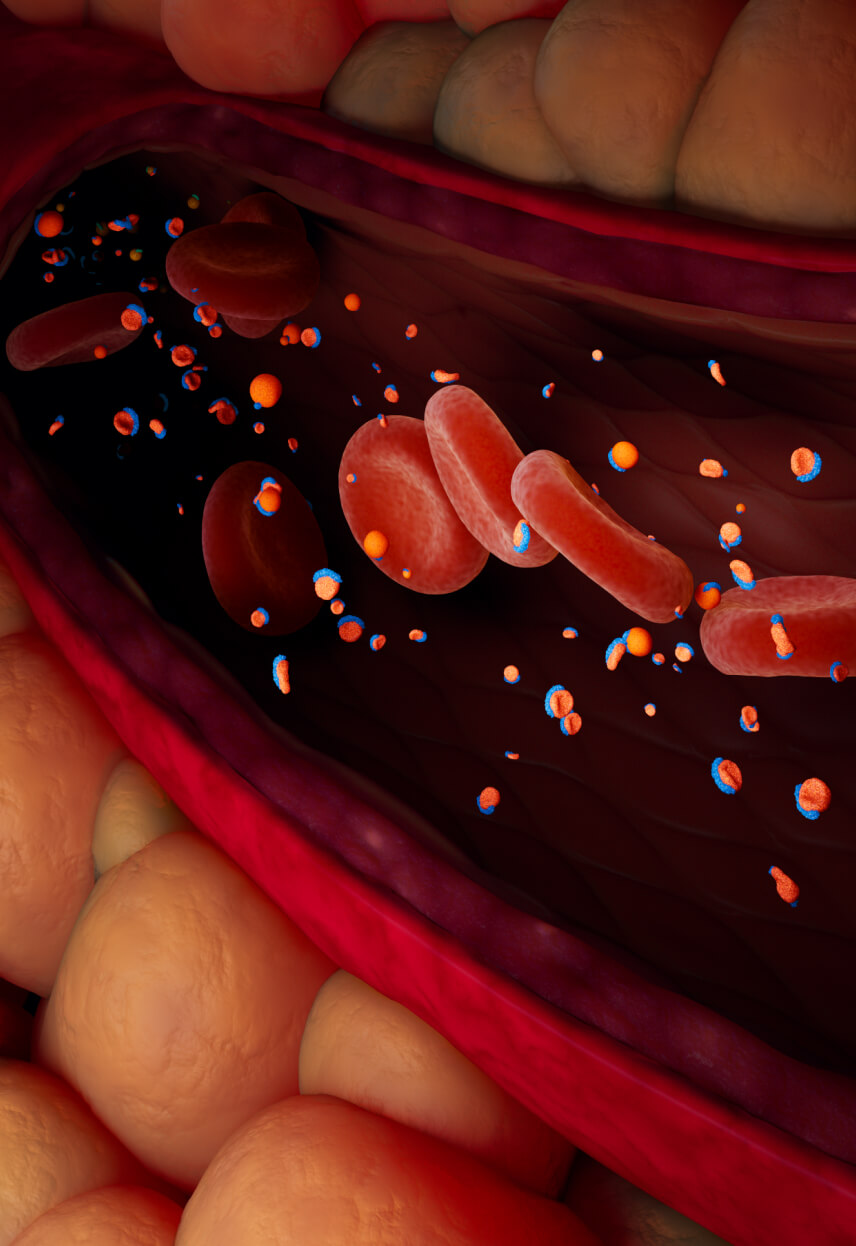
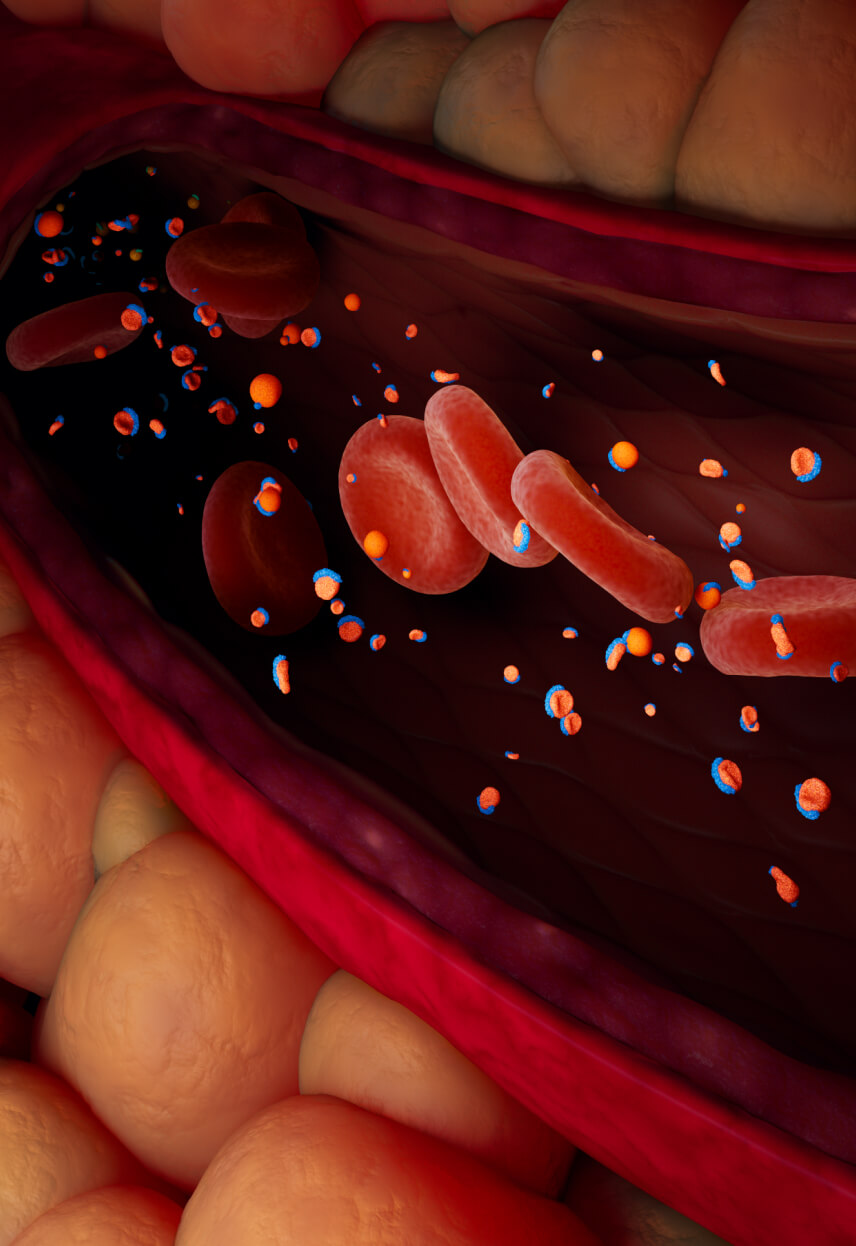
When plasma TG levels are optimal (<~1.2 mmol/L (~100 mg/dL), TRL remnant particles are cleared in the
liver and may be undetectable in the blood.1
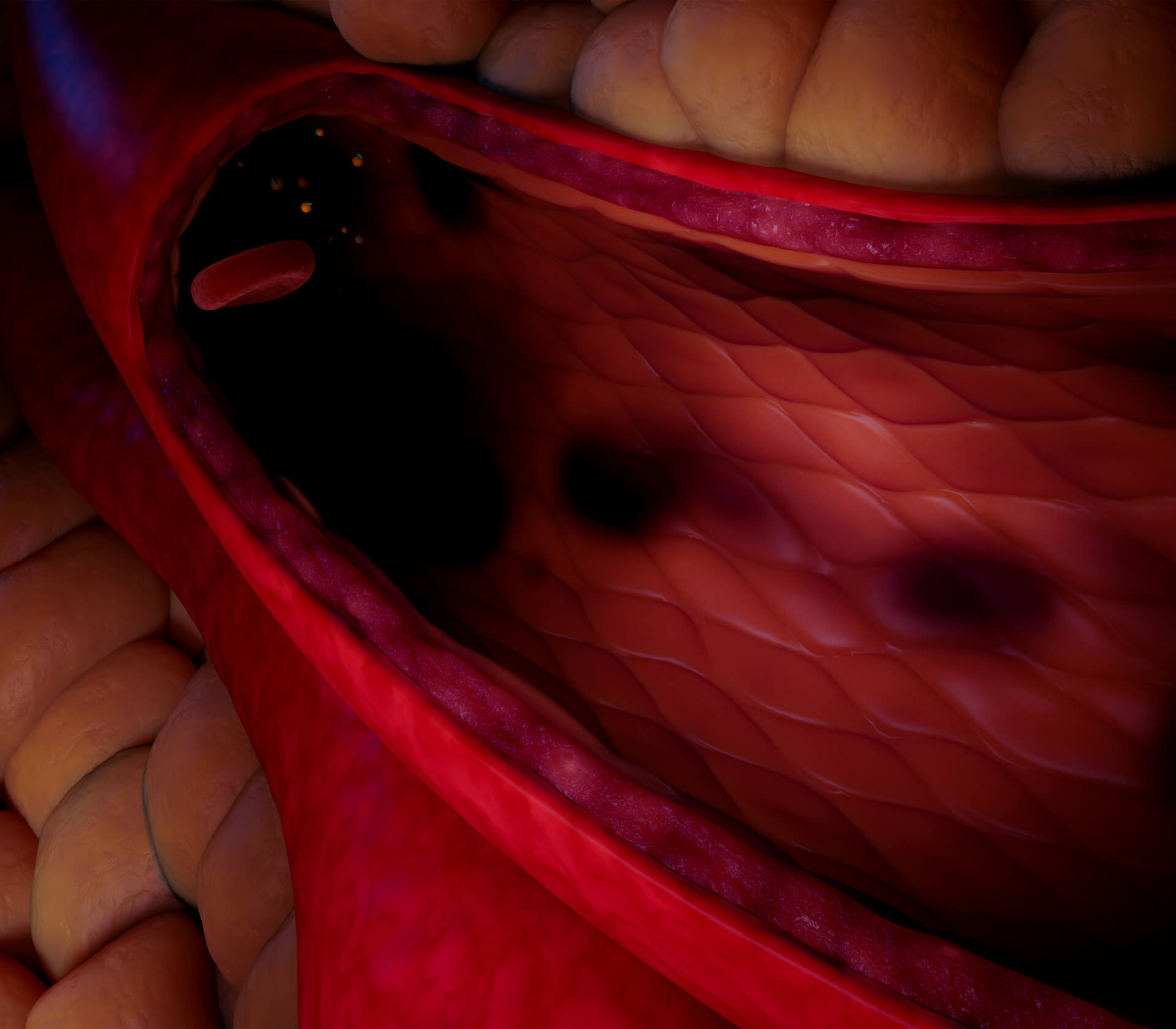
TRL remnants
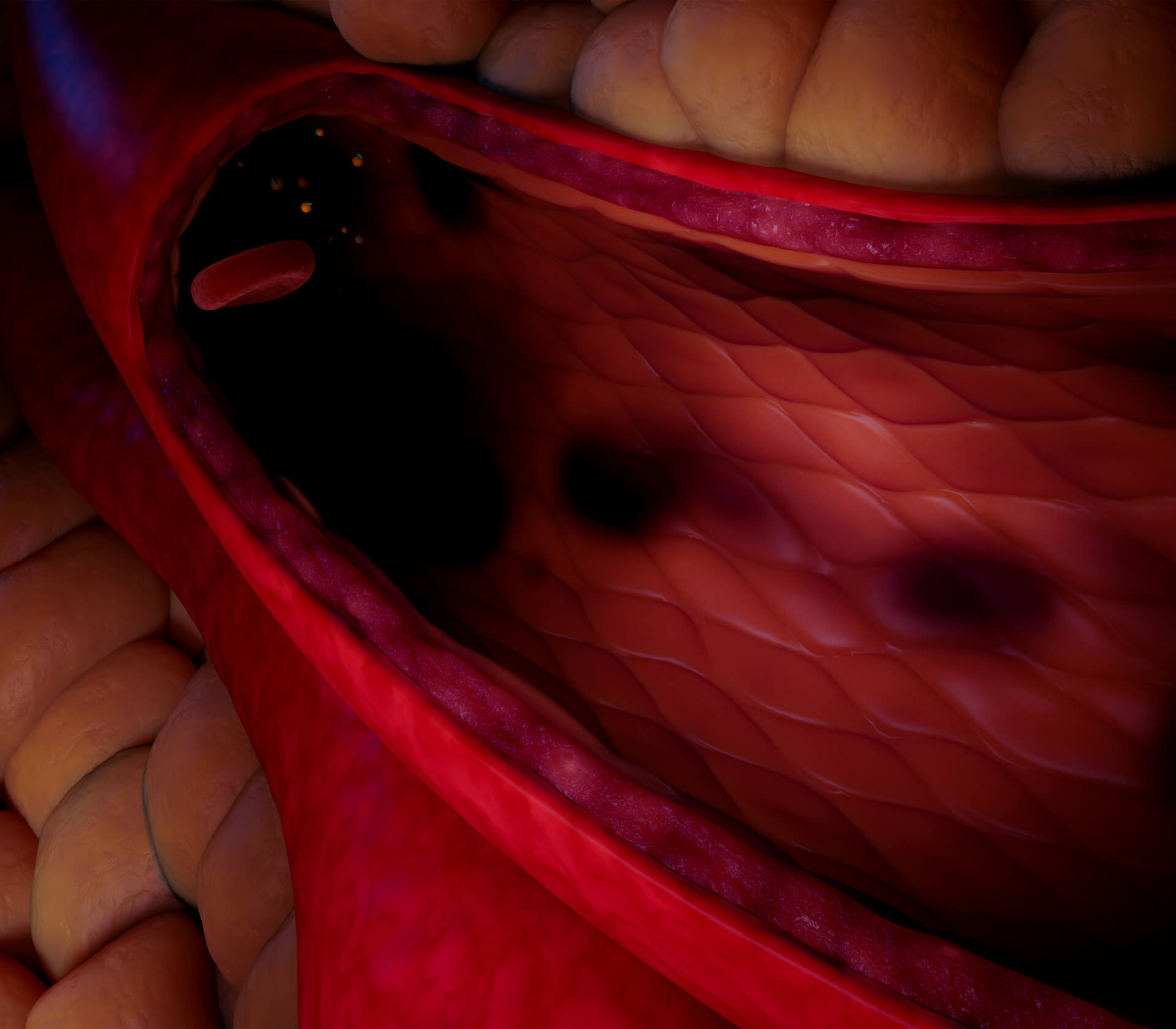
When TG levels are moderately elevated (>1.5 mmol/L (~150 mg/dL), there is increased VLDL secretion from
the liver and chylomicrons from the small intestines.
Furthermore, LPL is often impaired, especially in conditions such as obesity, insulin resistance, or
diabetes mellitus.
These effects lead to accumulation of TRL remnants in the blood.1
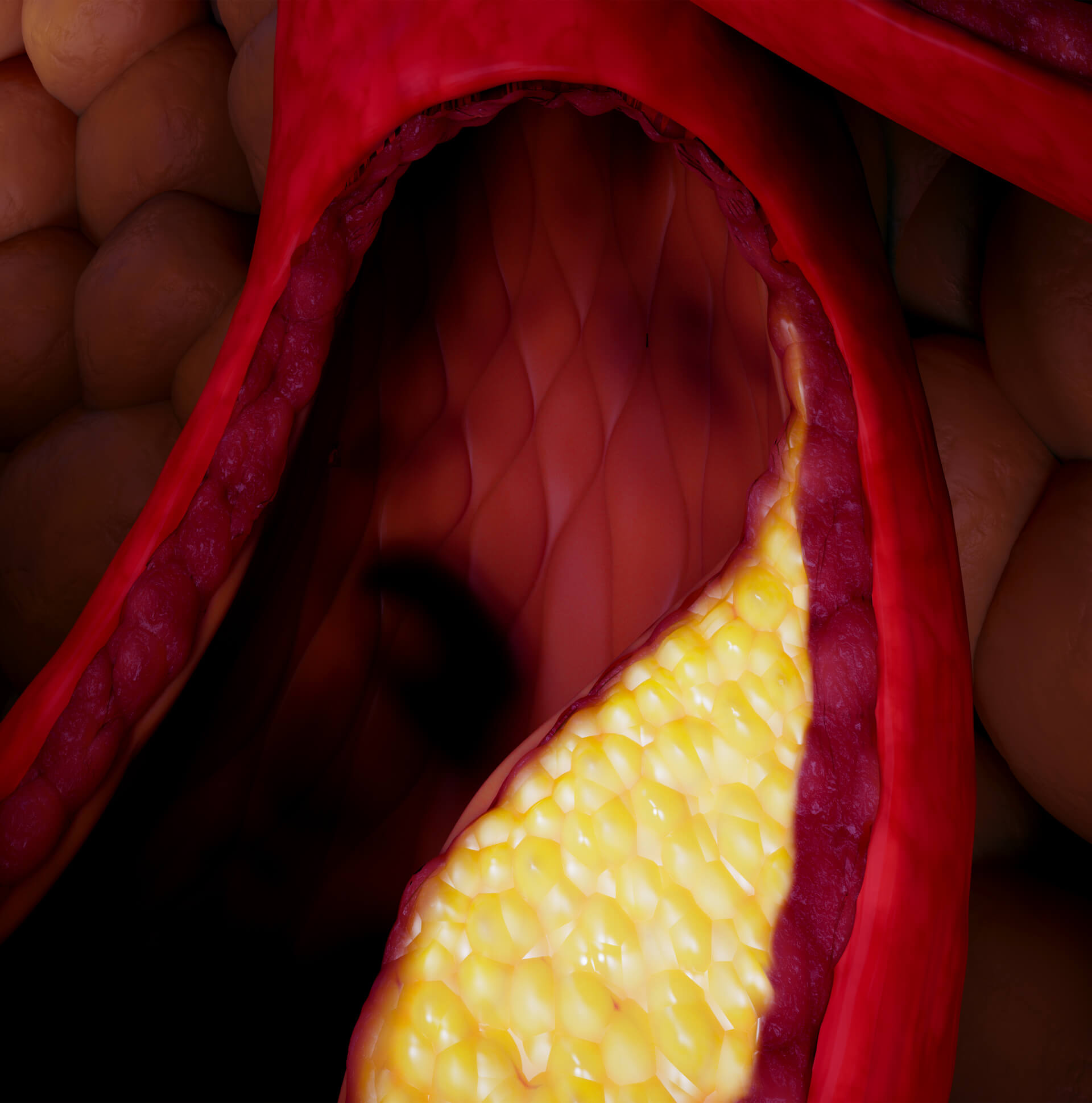
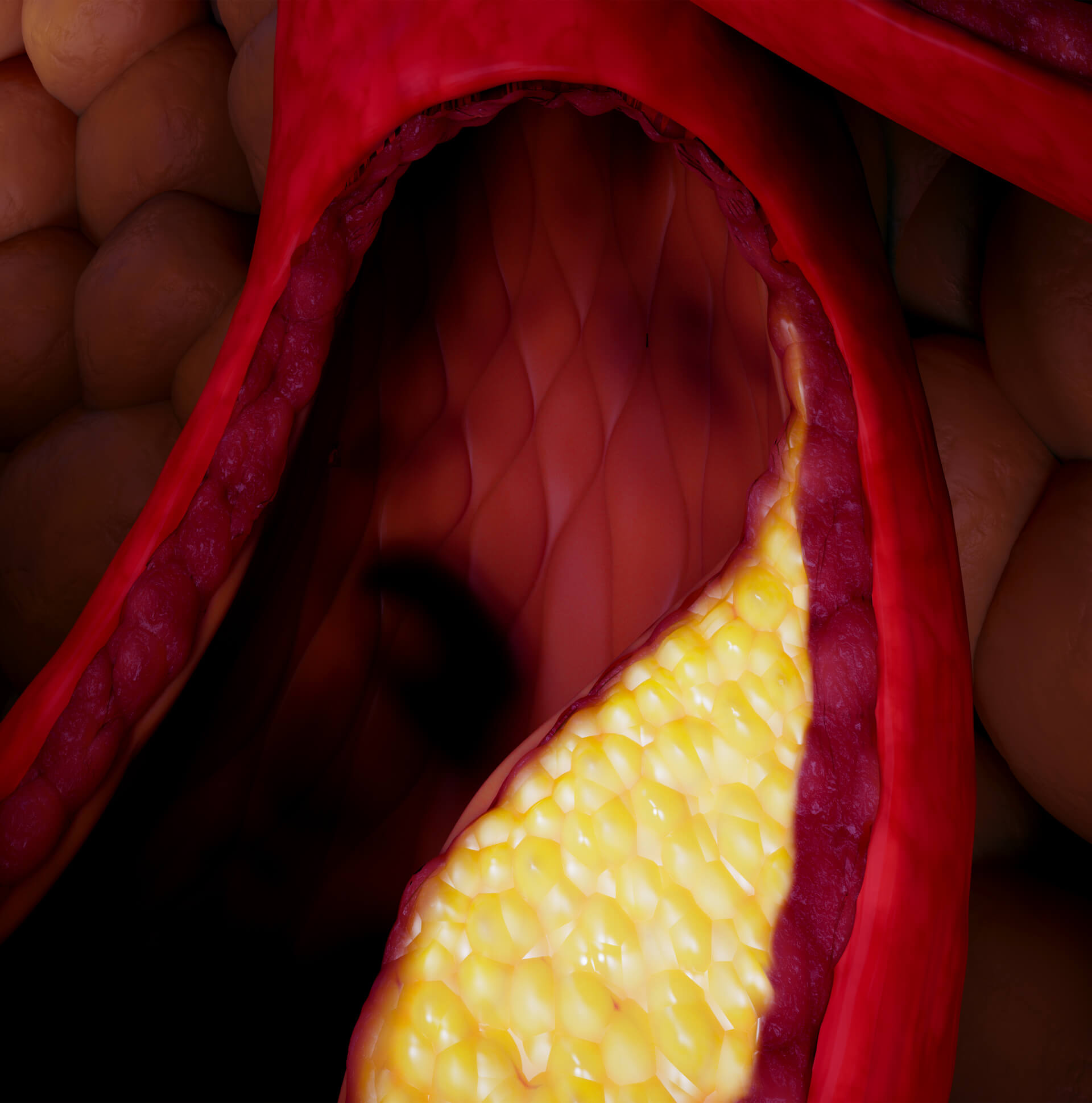
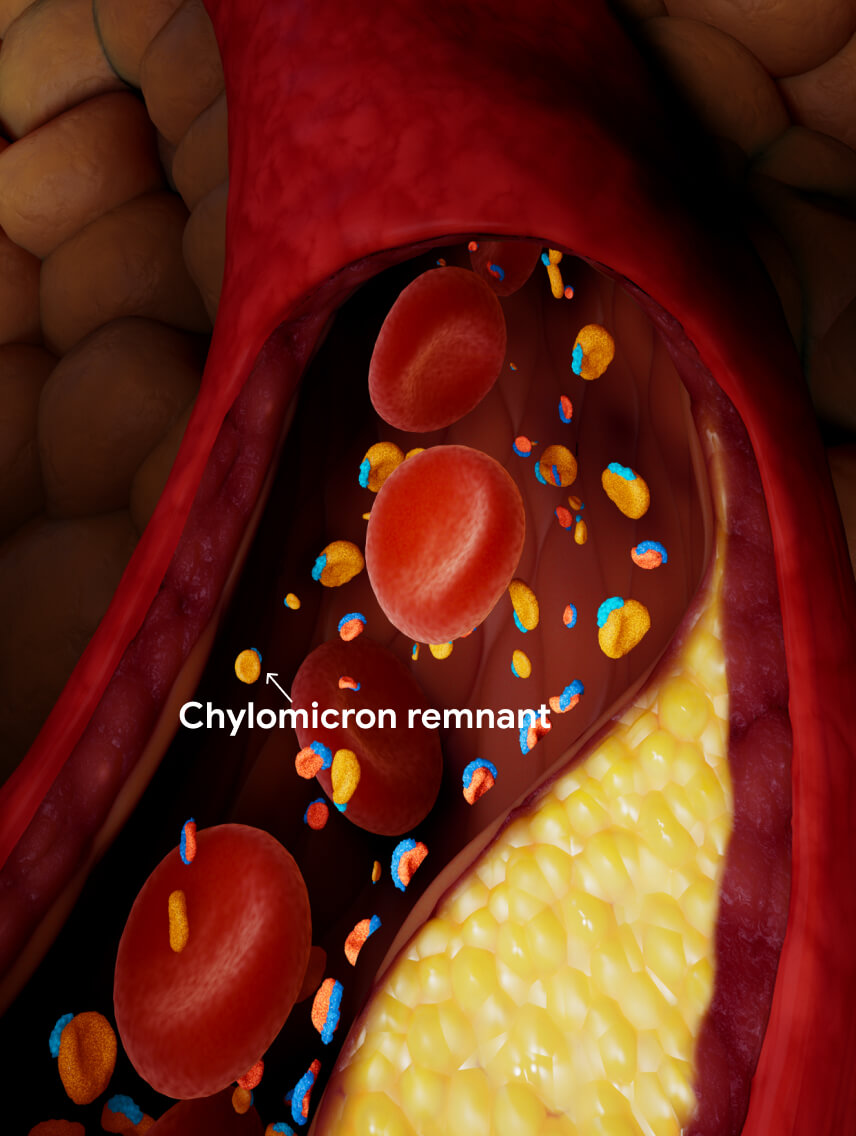
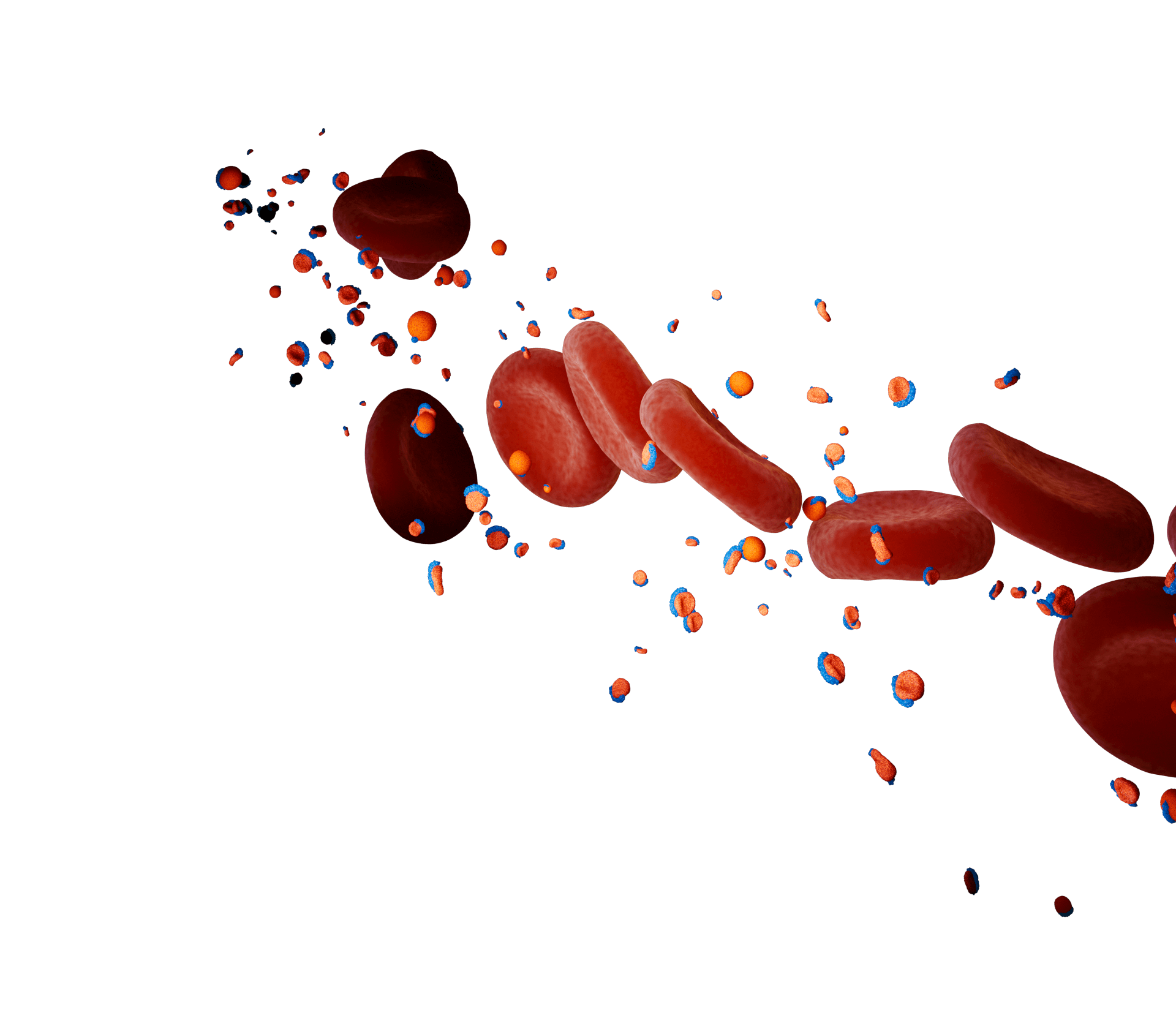
TRL remnants contribute to the initiation and progression of atherosclerotic
lesions.1
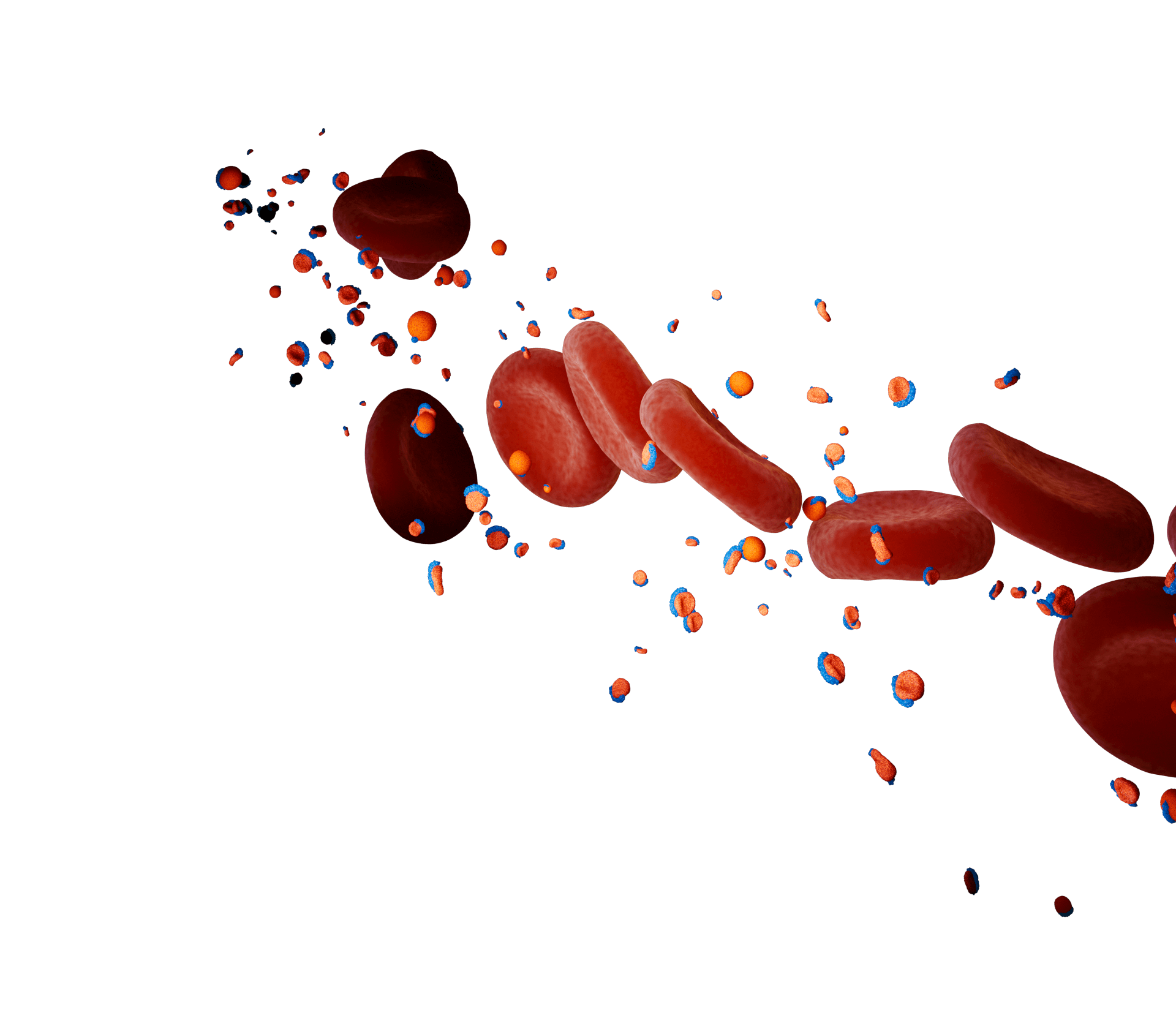
In some cases of extreme HTG, such as in the monogenic familial chylomicronemia syndrome (FCS),
clearance of chylomicrons from the bloodstream is impaired leading to chylomicronemia.14
Chylomicron remnant
The main TRLs in the blood are chylomicrons and very-low-density lipoproteins (VLDL).1,4
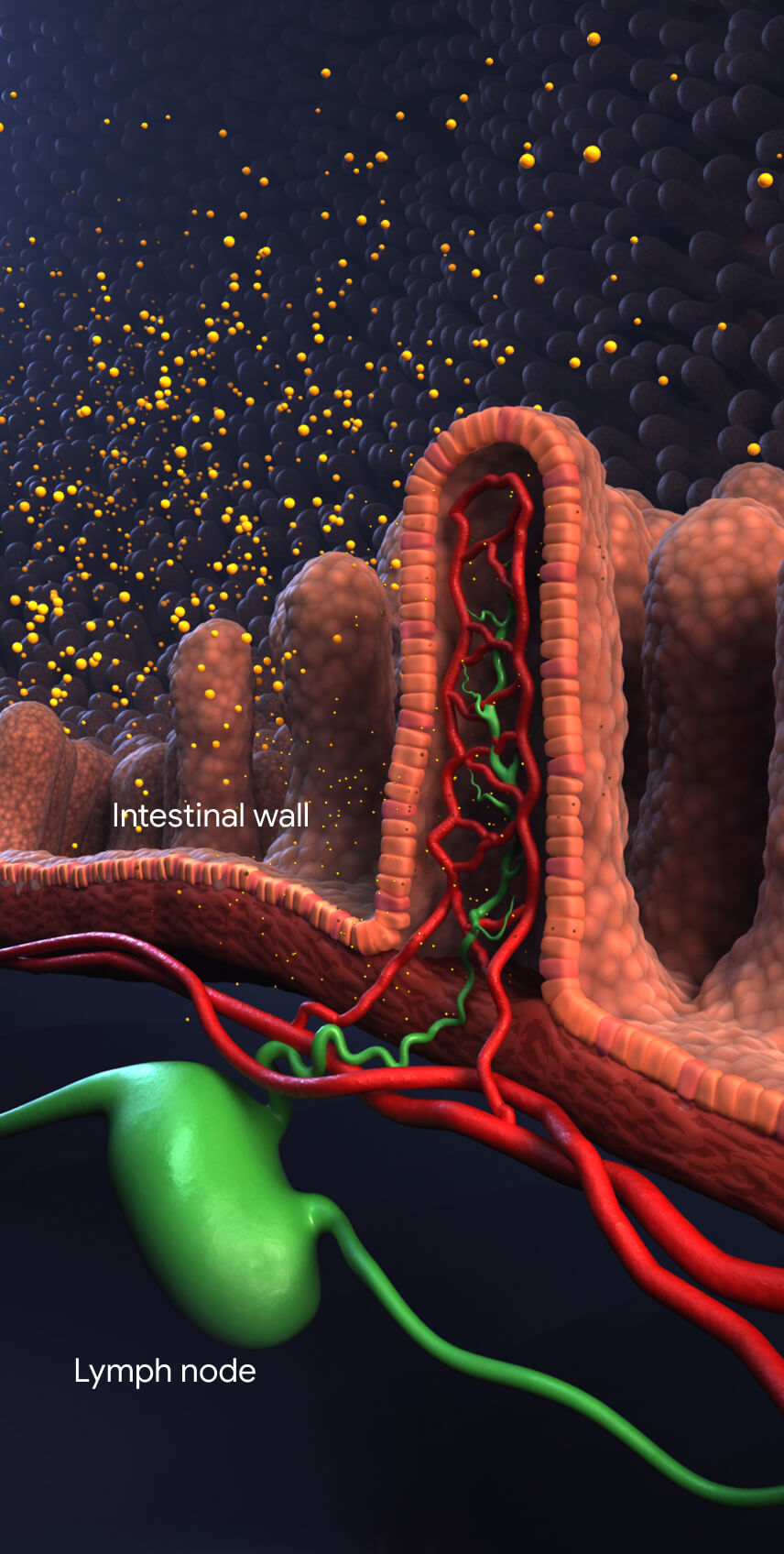
Chylomicrons are synthesized from dietary fats by intestinal enterocytes. They enter the bloodstream through
the lymphatic system.14,16
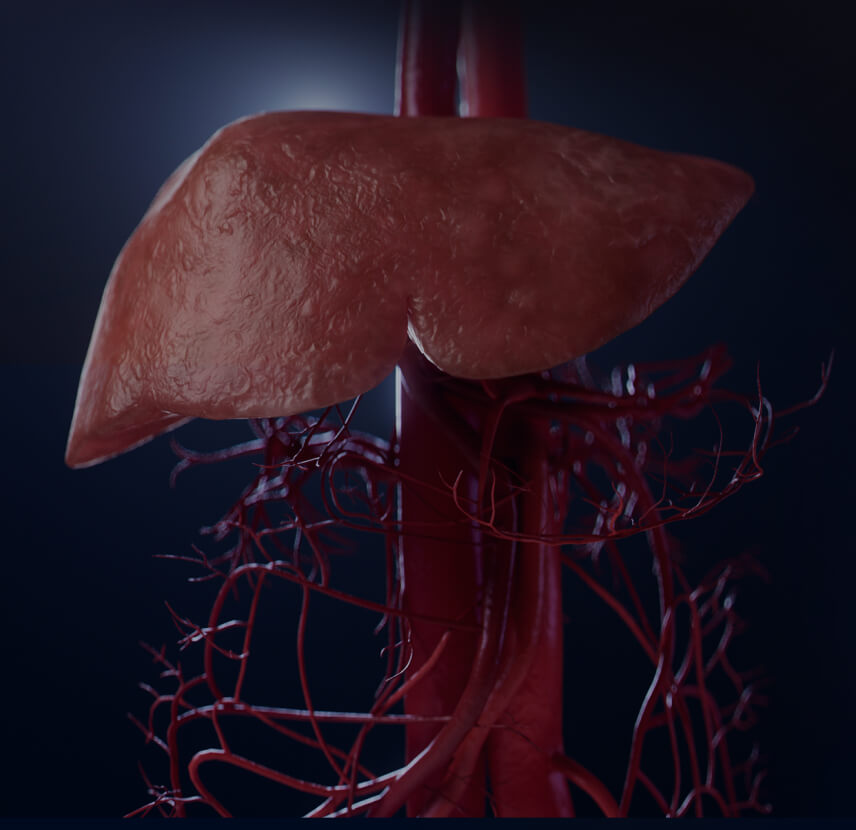
VLDL are made in the liver and secreted directly into the bloodstream.4
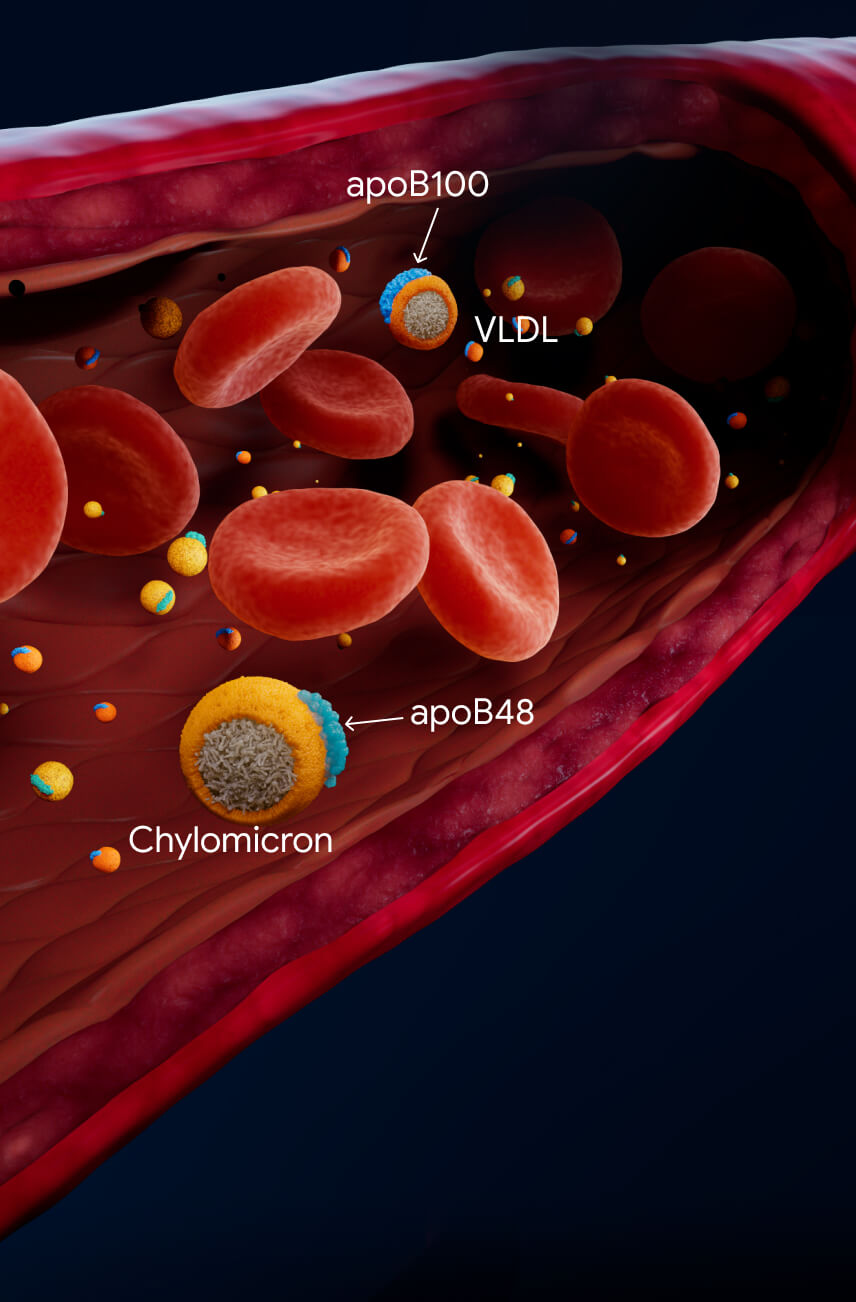
Chylomicrons and VLDL transport triglycerides in the bloodstream.1
In muscle and adipose tissues, endothelial cells express lipoprotein lipase (LPL) on their
surface.16
When plasma TG levels are optimal (<~1.2 mmol/L (~100 mg/dL), TRL remnant particles are cleared in the liver
and may be undetectable in the blood.1
TG lipolysis mediated by LPL usually clears chylomicrons from the bloodstream within 3-4 hours after a
meal.1,16 LPL also lipolyzes TGs from VLDL leaving TRL remnant particles, intermediate-density lipoproteins
(IDL), and small, dense low-density lipoproteins (LDL).1
TRL remnants contribute to the initiation and progression of atherosclerotic lesions.1
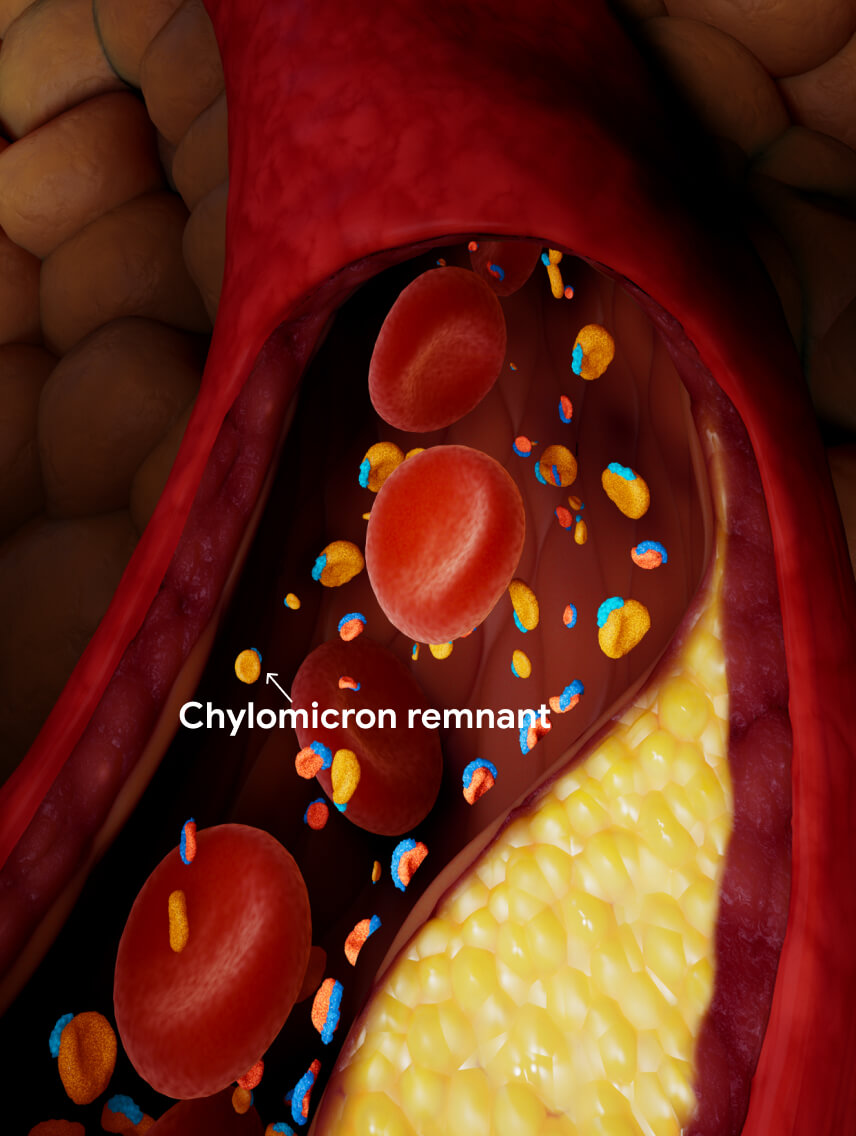
In some cases of extreme HTG, such as in the monogenic familial chylomicronemia syndrome (FCS), clearance of
chylomicrons from the bloodstream is impaired leading to chylomicronemia.14