Patient profiles
Managing severe hypertriglyceridemia (sHTG) starts with prompt patient identification
Choose a patient journey to explore

She experienced her first AP attack. Will there be another?

His diabetes and triglycerides were out of control.

His cardiologist suspected there was more to his sHTG.

When the standard of care isn't working, it's time to dig deeper.
Not real patients; actor portrayals and generated models.

Sandra, 49
Has sHTG with a history of acute pancreatitis (AP)
Not a real patient; actor portrayal or generated model.- Diagnosed with sHTG at 47 (fasting TGs of 664 mg/dL and 773 mg/dL)
- Started on a fibrate but stopped due to myalgias
- AP event at 48
- Was prescribed omega-3 fatty acid and a statin along with lifestyle modifications, but TGs remained ≥500 mg/dL
- Remains anxious about another AP event if TGs aren't lowered significantly
- Diagnosed with sHTG at 47 (fasting TGs of 664 mg/dL and 773 mg/dL)
- Started on a fibrate but stopped due to myalgias
- AP event at 48
- Was prescribed omega-3 fatty acid and a statin along with lifestyle modifications, but TGs remained ≥500 mg/dL
- Remains anxious about another AP event if TGs aren't lowered significantly

Lawrence, 62
Has sHTG and type 2 diabetes mellitus (T2DM)
Not a real patient; actor portrayal or generated model.- Under the care of an endocrinologist for diabetes and on metformin for many years
- Recently started on a statin and lifestyle modifications to lower TGs
- A1c improved but TGs persisted in the range of 789 mg/dL to 873 mg/dL (fasting)
- Was prescribed omega-3 fatty acid, and later a fibrate, but TGs remained ≥500 mg/dL
- Was prescribed a GLP-1 receptor agonist, which achieved weight loss and better glycemic control but showed limited TG reduction
- Worries his endocrinologist won't find a more effective therapy to lower his TGs adequately, leaving him at risk for AP
- Under the care of an endocrinologist for diabetes and on metformin for many years
- Recently started on a statin and lifestyle modifications to lower TGs
- A1c improved but TGs persisted in the range of 789 mg/dL to 873 mg/dL (fasting)
- Was prescribed omega-3 fatty acid, and later a fibrate, but TGs remained ≥500 mg/dL
- Was prescribed a GLP-1 receptor agonist, which achieved weight loss and better glycemic control but showed limited TG reduction
- Worries his endocrinologist won't find a more effective therapy to lower his TGs adequately, leaving him at risk for AP

Michael, 58
Has sHTG and hypertension, and was diagnosed with multifactorial chylomicronemia syndrome (MCS)
Not a real patient; actor portrayal or generated model.- Has been on an ACE inhibitor for hypertension, and a statin
- Fasting TGs 650 mg/dL
- Cardiologist prescribed strict diet
- Complained of intermittent abdominal discomfort and difficulty adhering to the diet at 6-week follow-up
- Repeat lipid panel showed TG level of 1500 mg/dL (fasting)
- Started on an omega-3 fatty acid, and later a fibrate, but TGs remained >880 mg/dL
- Cardiologist used NAFCS scoring tool to rule out FCS, a monogenic genetic form of sHTG10,11
- Was diagnosed with MCS, a polygenic form of sHTG, commonly seen with comorbid conditions11,12
It’s time to make a change."
- Has been on an ACE inhibitor for hypertension, and a statin
- Fasting TGs 650 mg/dL
- Cardiologist prescribed strict diet
- Complained of intermittent abdominal discomfort and difficulty adhering to the diet at 6-week follow-up
- Repeat lipid panel showed TG level of 1500 mg/dL (fasting)
- Started on an omega-3 fatty acid, and later a fibrate, but TGs remained >880 mg/dL
- Cardiologist used NAFCS scoring tool to rule out FCS, a monogenic genetic form of sHTG10,11
- Was diagnosed with MCS, a polygenic form of sHTG, commonly seen with comorbid conditions11,12
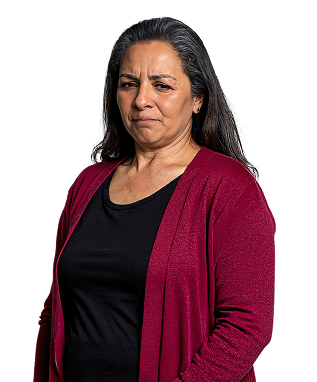
Maria, 53
Has sHTG
Not a real patient; actor portrayal or generated model.- Fasting TGs of 863 mg/dL during routine physical exam with primary care doctor
- Repeat lipid panels show TG levels consistently ≥500 mg/dL
- Has been on an omega-3 fatty acid and committed to lifestyle modifications, which slightly reduced TGs, but they were still ≥500 mg/dL
- Started on a statin, and eventually a fibrate, but TGs remained ≥500 mg/dL
- Fasting TGs of 863 mg/dL during routine physical exam with primary care doctor
- Repeat lipid panels show TG levels consistently ≥500 mg/dL
- Has been on an omega-3 fatty acid and committed to lifestyle modifications, which slightly reduced TGs, but they were still ≥500 mg/dL
- Started on a statin, and eventually a fibrate, but TGs remained ≥500 mg/dL
A1c=glycated hemoglobin; ACE inhibitor=angiotensin-converting enzyme inhibitor; AP=acute pancreatitis; ASCVD=atherosclerotic cardiovascular disease; BMI=body mass index; FCS=familial chylomicronemia syndrome; GLP-1=glucagon-like peptide-1; NAFCS=North American Familial Chylomicronemia Syndrome; TG=triglyceride.
References
References
-
Virani SS, Morris PB, Agarwala A, et al. 2021 ACC expert consensus decision pathway on the management of ASCVD risk reduction in patients with persistent hypertriglyceridemia: a report of the American College of Cardiology solution set oversight committee. J Am Coll Cardiol. 2021;78(9):960-993.
-
Nawaz H, Koutroumpakis E, Easler J, et al. Elevated serum triglycerides are independently associated with persistent organ failure in acute pancreatitis. Am J Gastroenterol. 2015;110(10):1497-1503.
-
Yuan G, Al-Shali KZ, Hegele RA. Hypertriglyceridemia: its etiology, effects and treatment. CMAJ. 2007;176(8):1113-1120.
-
Rashid N, Sharma PP, Scott RD, Lin KJ, Toth PP. Severe hypertriglyceridemia and factors associated with acute pancreatitis in an integrated health care system. J Clin Lipidol. 2016;10(4):880-890.
-
Sanchez RJ, Ge W, Wei W, Ponda MP, Rosenson RS. The association of triglyceride levels with the incidence of initial and recurrent acute pancreatitis. Lipids Health Dis. 2021;20(1):72.
-
Patel SB, Wyne KL, Afreen S, et al. American Association of Clinical Endocrinology clinical practice guideline on pharmacologic management of adults with dyslipidemia. Endocr Pract. 2025;31(2):236-262.
-
Skulas-Ray AC, Wilson PWF, Harris WS, et al. Omega-3 fatty acids for the management of hypertriglyceridemia: a science advisory from the American Heart Association. Circulation. 2019;140(12):e673-e691.
-
Hegele RA, Ahmad Z, Ashraf A, et al. Development and validation of clinical criteria to identify familial chylomicronemia syndrome (FCS) in North America. J Clin Lipidol. 2025;19(1)(online-only supplementary material):83-94.
-
Rivera FB, Chin MNC, Pine PLS, et al. Glucagon-like peptide 1 receptor agonists modestly reduced low-density lipoprotein cholesterol and total cholesterol levels independent of weight reduction: a meta-analysis and meta-regression of placebo controlled randomized controlled trials. Curr Med Res Opin. 2025;41(1):185-197.
-
Hegele RA, Ahmad Z, Ashraf A, et al. Development and validation of clinical criteria to identify familial chylomicronemia syndrome (FCS) in North America. J Clin Lipidol. 2025;19(1):83-94.
-
Paquette M, Bernard S. The evolving story of multifactorial chylomicronemia syndrome. Front Cardiovasc Med. 2022;9:886266.
-
Moulin P, Dufour R, Averna M, et al. Identification and diagnosis of patients with familial chylomicronaemia syndrome (FCS): expert panel recommendations and proposal of an "FCS score". Atherosclerosis. 2018;275:265-272.