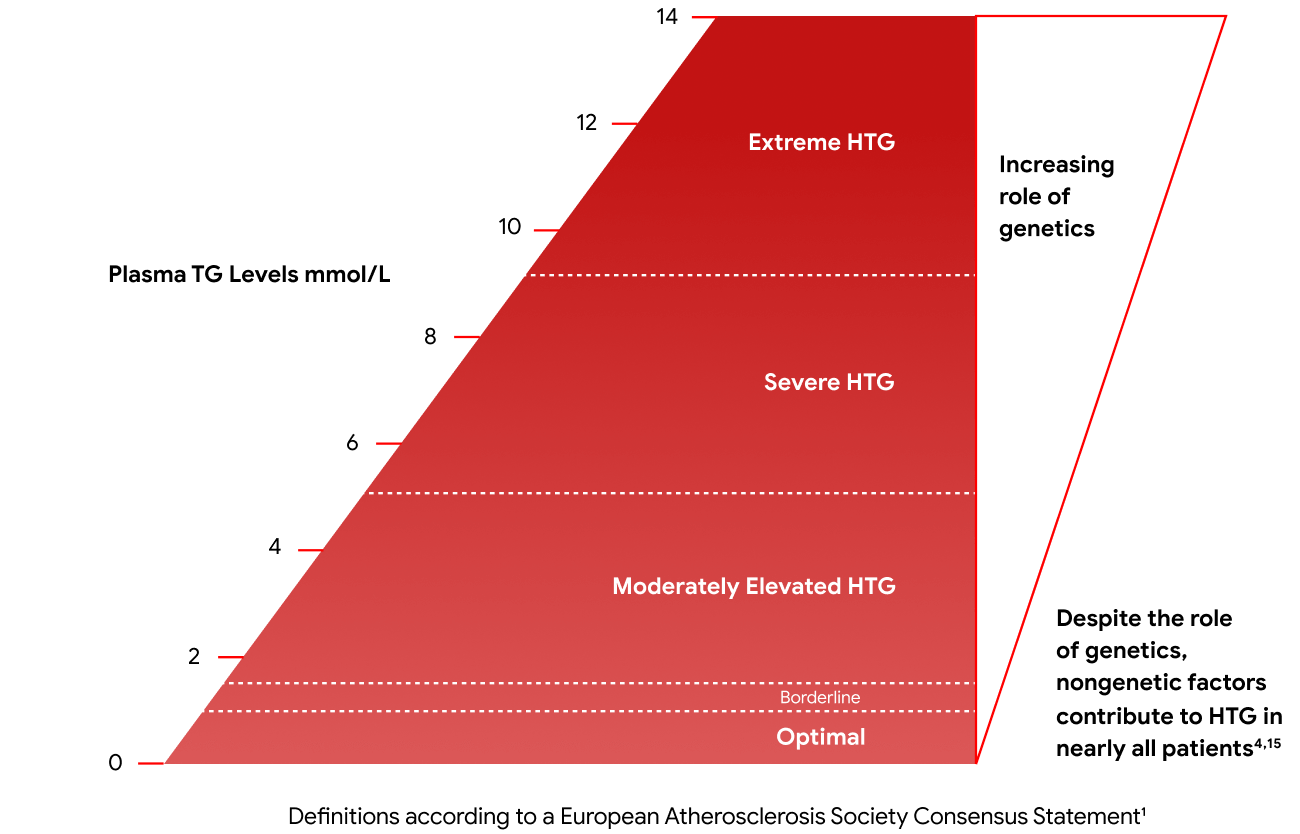
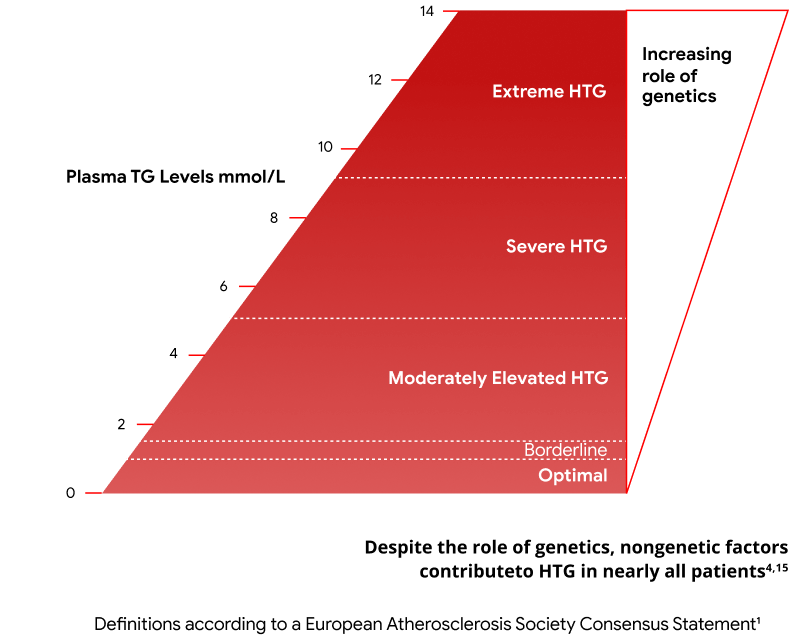
1. Ginsberg HN, Packard CJ, Chapman MJ, et al. Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European Atherosclerosis Society. Eur Heart J. 2021;42(47):4791-4806.
2. Virani SS, Morris PB, Agarwala A, et al. 2021 ACC Expert Consensus Decision Pathway on the Management of ASCVD Risk Reduction in Patients With Persistent Hypertriglyceridemia: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021.
3. Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626-635.
4. Laufs U, Parhofer KG, Ginsberg HN, et al. Clinical review on triglycerides. Eur Heart J. 2020;41(1):99-109c.
5. Packard CJ. Remnants, LDL, and the Quantification of Lipoprotein-Associated Risk in Atherosclerotic Cardiovascular Disease. Curr Atheroscler Rep. 2022;24(1534-6242 (Electronic)):133-142.
6. Wang Y. Higher fasting triglyceride predicts higher risks of diabetes mortality in US adults. Lipids Health Dis. 2021;20(1):181.
7. Paquette M, Bernard S. The Evolving Story of Multifactorial Chylomicronemia Syndrome. Front Cardiovasc Med. 2022;9:886266.
8. Christian JB, Bourgeois N, Snipes R, et al. Prevalence of severe (500 to 2,000 mg/dl) hypertriglyceridemia in United States adults. Am J Cardiol. 2011;107(6):891-897.
9. Sandesara PB, Virani SS, Fazio S, et al. The Forgotten Lipids: Triglycerides, Remnant Cholesterol, and Atherosclerotic Cardiovascular Disease Risk. Endocr Rev. 2019;40(2):537-557.
10. Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting Mild-to-Moderate Hypertriglyceridemia and Risk of Acute Pancreatitis. JAMA Intern Med. 2016;176(12):1834-1842.
11. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111-188.
12. Chyzhyk V, Brown AS. Familial chylomicronemia syndrome: A rare but devastating autosomal recessive disorder characterized by refractory hypertriglyceridemia and recurrent pancreatitis. Trends Cardiovasc Med. 2020;30(2):80-85.
13. Santos-Baez LS, Ginsberg HN. Hypertriglyceridemia-Causes, Significance, and Approaches to Therapy. Front Endocrinol (Lausanne). 2020;11:616.
14. Moulin P, Dufour R, Averna M, et al. Identification and diagnosis of patients with familial chylomicronaemia syndrome (FCS): Expert panel recommendations and proposal of an "FCS score". Atherosclerosis. 2018;275:265-272.
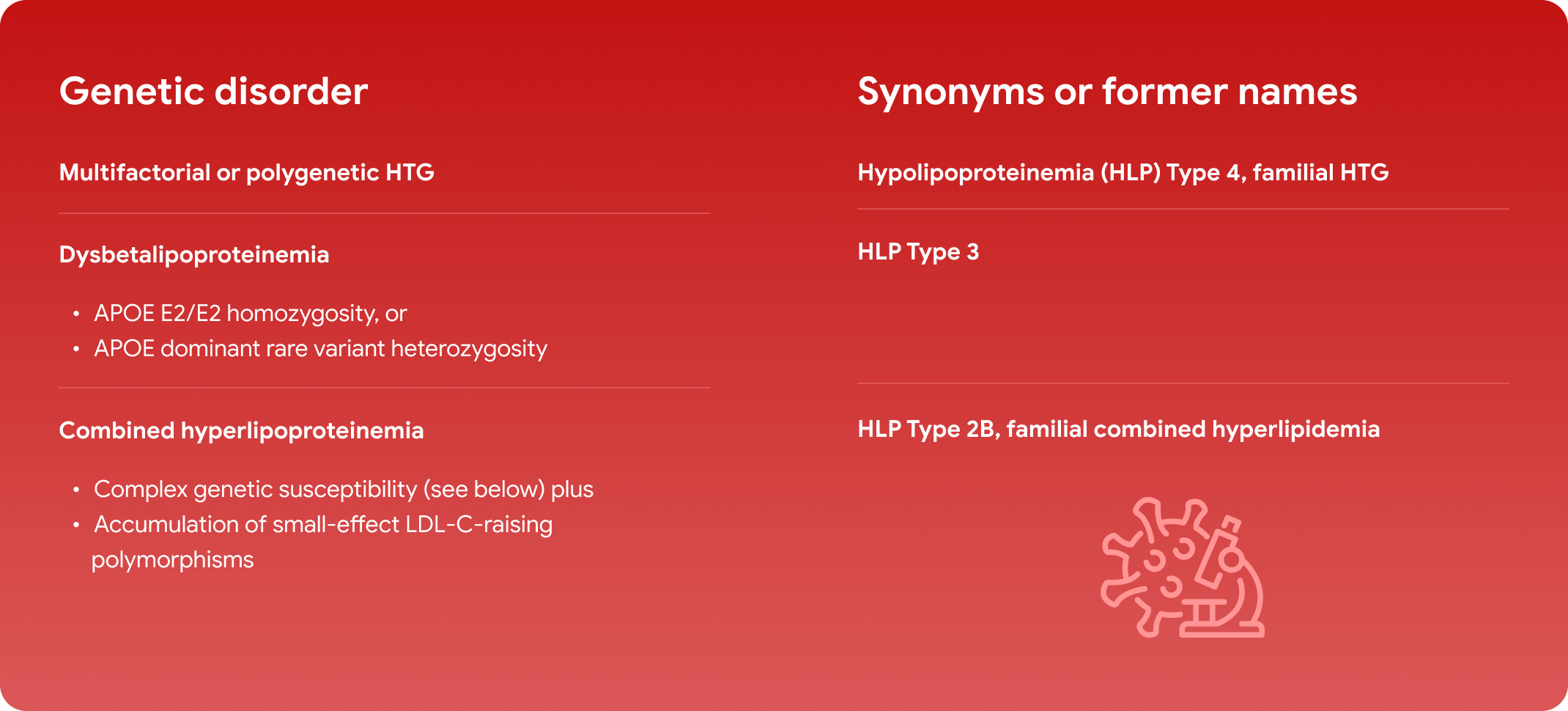
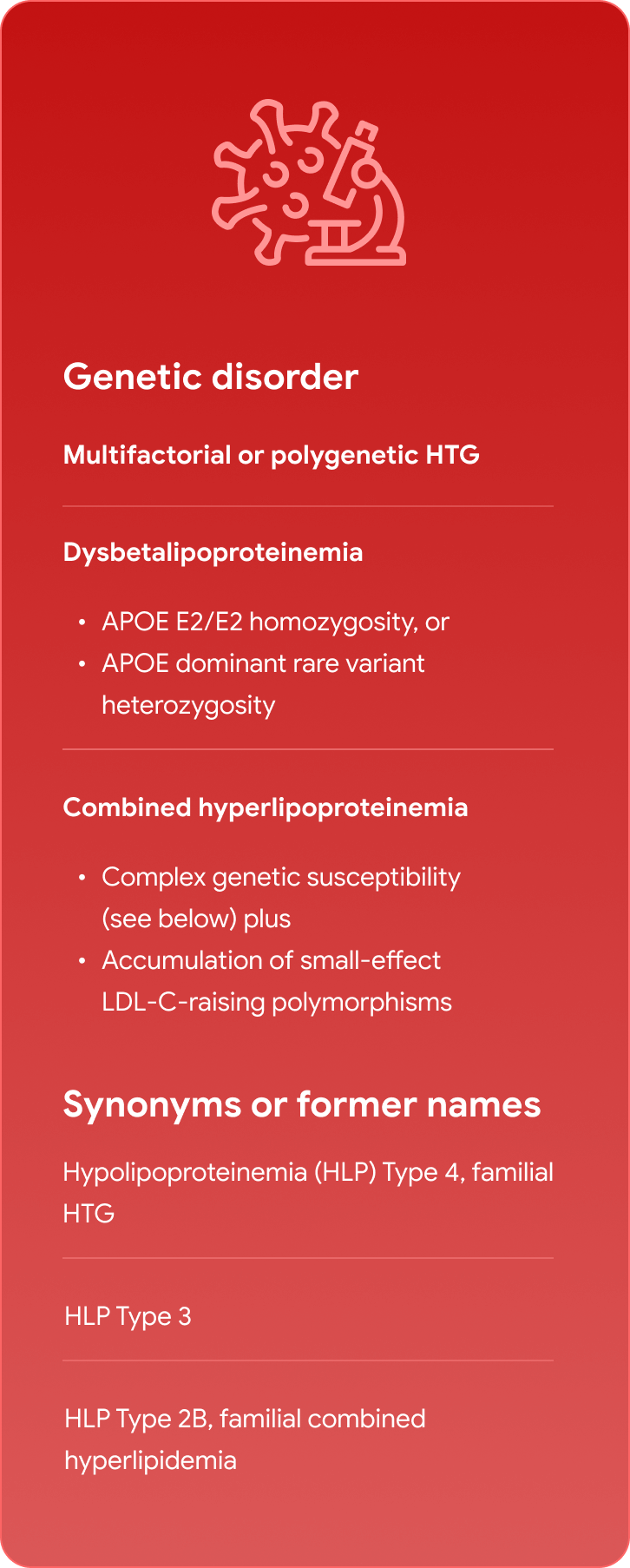
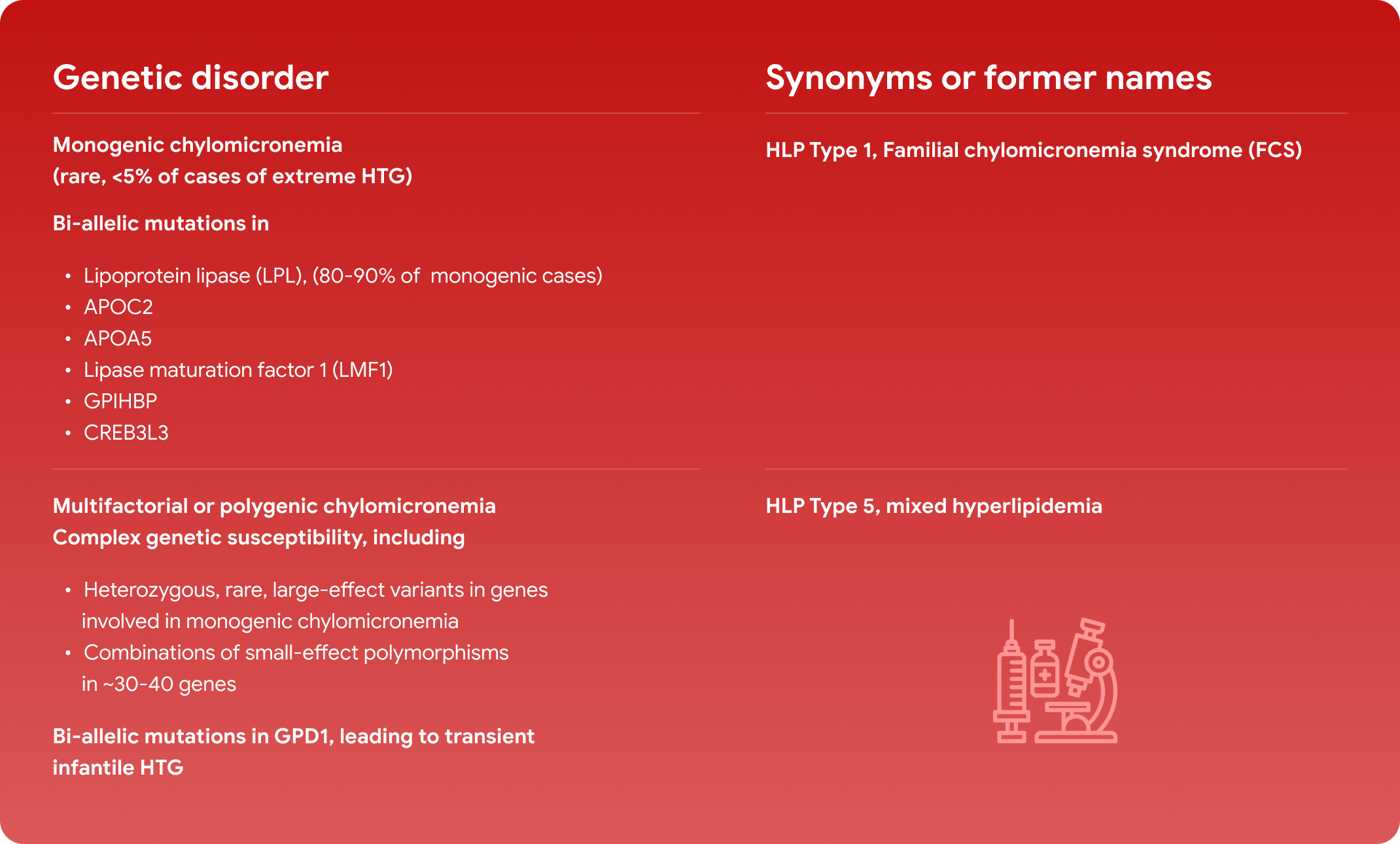
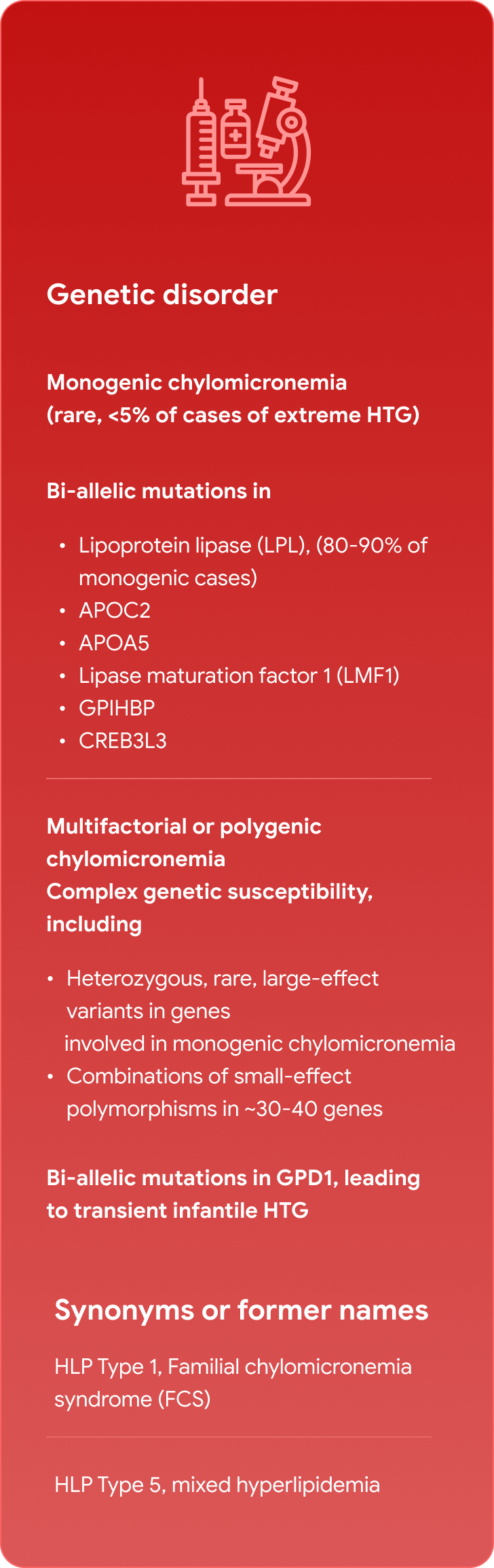
15. Hegele RA, Ginsberg HN, Chapman MJ, et al. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2(8):655-666.
16. Brahm AJ, Hegele RA. Chylomicronaemia--current diagnosis and future therapies. Nat Rev Endocrinol. 2015;11(6):352-362.
17. Borén J, Chapman MJ, Krauss RM, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41(24):2313-2330.
18. Semenkovich CF. Disorder of Lipid Metabolism. In: Goldman LaS, A.I., editor. Goldman-Cecil Medicine, 25th Edition. Philadelphia, PA: Elsevier Saunders; 2016. p. 1389-1397.
19. Nordestgaard BG. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease: New Insights From Epidemiology, Genetics, and Biology. Circ Res. 2016;118(4):547-563.
20. Nordestgaard BG, Benn M, Schnohr P, et al. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. Jama. 2007;298(3):299-308.
21. Stroes E, Moulin P, Parhofer KG, et al. Diagnostic algorithm for familial chylomicronemia syndrome. Atheroscler Suppl. 2017;23:1-7.
22. Davidson M, Stevenson M, Hsieh A, et al. The burden of familial chylomicronemia syndrome: Results from the global IN-FOCUS study. J Clin Lipidol. 2018;12(4):898-907.e892.
23. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285-e350.
24. Belhassen M, Van Ganse E, Nolin M, et al. 10-Year Comparative Follow-up of Familial versus Multifactorial Chylomicronemia Syndromes. J Clin Endocrinol Metab. 2021;106(3):e1332-e1342.
25. Nawaz H, Koutroumpakis E, Easler J, et al. Elevated serum triglycerides are independently associated with persistent organ failure in acute pancreatitis. Am J Gastroenterol. 2015;110(10):1497-1503.
26. Bedogni G, Bellentani S, Miglioli L, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33.
27. Koehler EM, Schouten JN, Hansen BE, et al. External validation of the fatty liver index for identifying nonalcoholic fatty liver disease in a population-based study. Clin Gastroenterol Hepatol. 2013;11(9):1201-1204.
28. Nivukoski U, Niemelä M, Bloigu A, et al. Combined effects of lifestyle risk factors on fatty liver index. BMC Gastroenterol. 2020;20(1):109.
29. Maltais M, Brisson D, Gaudet D. Non-Alcoholic Fatty Liver in Patients with Chylomicronemia. J Clin Med. 2021;10(4).
30. O'Dea LSL, MacDougall J, Alexander VJ, et al. Differentiating Familial Chylomicronemia Syndrome From Multifactorial Severe Hypertriglyceridemia by Clinical Profiles. J Endocr Soc. 2019;3(12):2397-2410.
31. Handelsman Y, Jellinger PS, Guerin CK, Bloomgarden ZT, Brinton EA, Budoff MJ, Davidson MH, Einhorn D, Fazio S, Fonseca VA, Garber AJ, Grunberger G, Krauss RM, Mechanick JI, Rosenblit PD, Smith DA, Wyne KL. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Management of Dyslipidemia and Prevention of Cardiovascular Disease Algorithm - 2020 Executive Summary. Endocr Pract. 2020;26(10):1196-224.
32. Hopkins PN, Wu LL, Hunt SC, Brinton EA. Plasma triglycerides and type III hyperlipidemia are independently associated with premature familial coronary artery disease. J Am Coll Cardiol. 2005;45(7):1003-12.
33. Toth PP, Grabner M, Ramey N, Higuchi K. Clinical and economic outcomes in a real-world population of patients with elevated triglyceride levels. Atherosclerosis. 2014;237(2):790-7.
34. Williams L, Rhodes KS, Karmally W, Welstead LA, Alexander L, Sutton L. Familial chylomicronemia syndrome: Bringing to life dietary recommendations throughout the life span. J Clin Lipidol. 2018;12(4):908-19.
35. ClinicalTrials.gov A Study of Olezarsen (ISIS 678354) in Participants With Hypertriglyceridemia and Atherosclerotic Cardiovascular Disease, or With Severe Hypertriglyceridemia. ClinicalTrials.gov identifier: NCT05610280. Accessed March 13, 2023. Updated March 1, 2023. https://clinicaltrials.gov/ct2/show/NCT05610280